증례보고: Karapandzic Flap을 사용한 하순부 재건
Case Report: Reconstruction of the Lower Lip using the Karapandzic Flap
Article information
Abstract
= Abstract =
Squamous cell carcinoma of the lip is a common malignant tumor originating from oral cancer. However, unlike other areas, the lips hold significant functional and aesthetic importance as a part of the face. As a result, a tailored approach based on the tumor’s size, type, and location is essential. The Karapandzic flap is especially suitable for reconstructing lesions located on the lip, particularly when the size of the cancer is large and other surgical treatments like free flaps are not feasible. It allows for extensive resection beyond the size of the lower lip. In this case, considering the patient’s overall condition, successful reconstruction of the lower lip was achieved using the Karapandzic flap.
Introduction
Squamous cell carcinoma (SCC) of the lip is a common malignant tumor, accounting for 25-30% of all oral cancers.1) It predominantly affects men over 50 years of age, with a male-to-female ratio of 6:1, especially those with prolonged sun exposure.2-3) As with other malignancies, excessive tobacco and alcohol consumption serve as contributory factors.3) While this tumor is exceedingly rare in younger individuals, cases have been reported in patients undergoing immunosuppressive therapy post-renal transplantation.4) When diagnosed early, the 5-year survival rate commonly surpasses 90%, offering an optimistic prognosis. However, a literature review paints a less rosy picture, suggesting lymph node metastasis in 5-20% of cases.3-5) The approach to reconstruction and prognosis can vary significantly based on several factors when squamous cell carcinoma of the lip is detected at a later stage. Late detection often accompanies more extensive tissue damage, complicating both reconstruction and prognosis. Multi-stage reconstruction or restorative surgical procedures may need to be employed even after the initial surgery. Compared to early detection, there can be impacts on recurrence rates, survival rates, and the quality of life. Reconstructive techniques for the lip differ from other facial regions, demanding meticulous attention both aesthetically and functionally in surgical intervention and subsequent management. Moreover, the post-surgical appearance can significantly impact the patient’s social interactions. In this case report, we report a successful removal and reconstruction of an SCC that pervaded the lip and provide a comprehensive literature review.
Case report
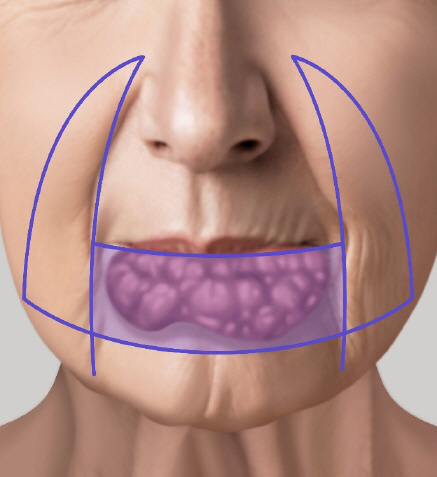
A 80-year-old male visited to the plastic surgery outpatient clinic with a mass on his lower lip. Accompanied by his son, who served as his caregiver due to the patient’s dementia, the patient had no recollection of his medical history (Fig. 1). According to the son, the mass had appeared a year prior and had gradually increased in size. It had expanded to encompass the entire lip a month before the visit. The patient was diagnosed with dementia three years before the presentation and had been on medication for it, as well as for hypertension and diabetes for 20 years. He had quit smoking five years prior. He had no previous history related to lip lesions and had never undergone surgery. Due to the progressive growth of the mass which caused persistent pain, difficulty speaking, and trouble eating, a biopsy was performed at a local hospital. The patient was diagnosed with squamous cell carcinoma (SCC) and was referred to our institution for surgical excision. The mass measured 8.5x3cm on the lower lip and was associated with pain and serous discharge. Before surgery, to determine cancer metastasis, a fine-needle aspiration and ultrasound were conducted. Heterogeneous lymphoid cells were detected in the neck region, prompting an otolaryngology intervention for a supra-omohyoid neck dissection, followed by a reconstruction in our department. Considering the patient’s underlying conditions, social background, and current dementia status, we opted for a local flap reconstruction rather than a free flap. The surgery was performed under general anesthesia. The surgery was first performed in the otolaryngology department. The spinal accessory nerve, internal jugular vein, and sternocleidomastoid muscle were preserved. On the right side, level I and II lymph node (LN) dissection was carried out, and on the left side, level I, II, and III LN dissection was performed. A resection was planned for the SCC alongside a Karapandzic flap (Fig. 2). Frozen section biopsies confirmed negative margins before the reconstructive procedure was conducted on the excised lower lip (Fig. 3). To prevent hematoma formation, a Hemo-vac drain was inserted in the neck region (Fig. 4). Ointment gauze dressings were frequently changed post-operatively to prevent drying of the surgical site. To minimize and restrict lip and peri-lip muscular movements, the patient was kept NPO for a week, receiving nutrition and antibiotics intravenously. The final pathology results indicated a well-differentiated Squamous cell carcinoma. There were no signs of lymphatic or vascular invasion, and among the 17 lymph nodes examined, no metastasis was confirmed. At the time of discharge, there were no signs of wound dehiscence, infection, hematoma, or secretions. The patient no longer complained of lip pain, difficulty in eating, or speaking challenges (Fig. 5).

Photograph of the patient before surgery. The squamous cell carcinoma covers the entirety of the lower lip.

TFrontal view of the patient after the reconstruction of the lower lip using the Karapandzic flap technique.
Discussion
The lips differ from other body parts as they perform various functions such as articulation, food intake, and facial expression.6) Consequently, their complex nature makes them crucial from both functional and aesthetic perspectives. The skin of the lips exhibits a layered structure; it begins as dry skin on the outer portion, transitions to a moist red hue towards the oral entrance, and becomes a mucous membrane inside the oral cavity.6-8) Lips receive their blood supply from the peripheral arteries emanating from the facial artery. The lower lip possesses a relatively simple aesthetic structure compared to the upper lip. It maintains a uniform contour, is more resilient, and typically has a greater tissue volume, making it feasible for use in reconstructing the upper lip.8) Any lip defects should account for the Cupid’s bow, philtral ridges, and alar margins. Both lips maintain adequate oral function through the muscles surrounding the commissures. Various reconstruction methods, from primary closure to the Abbe-Estlander flap and skin grafting, are considered based on defect size and location.8,9) Specifically, total lower lip reconstruction is a challenging procedure, achievable either via microsurgical free tissue transfer or multi-staged local flap repair. Both techniques have their merits and challenges, demanding specialized expertise.10) In this case report, we discuss a rare case involving the removal and reconstruction of an extensive squamous cell carcinoma (SCC) occupying more than two-thirds of the lip. A safety margin was included in the resection to prevent recurrence, making the actual resection significantly larger than the carcinoma itself. This necessitated the complete removal of the lower lip. In the operating room, a frozen biopsy confirmed the negative margin. Reconstruction was then performed using bilateral Karapandzic neurovascular rotation flaps. The Karapandzic flap is primarily used for large lip defects, particularly for the lower lip. This technique simultaneously transfers adjacent skin and muscles. It preserves sensation and motor function around the mouth, boasts a relatively higher flap survival rate, and ensures a harmonious aesthetic outcome in terms of skin color, texture, and thickness. While the option of a free flap was considered, given the patient’s smoking history, underlying conditions, vascular health, and desired aesthetic outcomes, the Karapandzic flap was deemed the optimal choice for reconstruction. A drawback of the Karapandzic flap is potential post-operative microstomia, which can complicate food intake. Additionally, it may introduce tension to the surrounding skin, heightening the risk of secondary com- plications. However, the functional, aesthetic, and social benefits outweigh these challenges. In conclusion, lip reconstruction following cancer requires a tailored approach, considering the patient’s overall health, cancer location and size, and patient expectations. Collaborative decision-making, involving plastic surgeons and head-neck specialists, is essential in selecting the most appropriate reconstructive method.