종격동내 위치한 갑상선 내 갑상설관 낭종: 증례 보고 및 문헌 고찰
Intrathyroid Thyroglossal Duct Cyst Extending into the Mediastinum: A Case Report and Review of Literature
Article information
Abstract
= Abstract =
Thyroglossal duct cyst (TGDC) is the most common congenital cyst in the neck and usually presents in children. It is most commonly located at the infrahyoid level. However, intrathyroid TGDC in the adult is extremely rare and its pathogenesis remains unclear. Curiously, an intrathyroid TGDC was found on the lateral aspect of the inferior pole of the thyroid gland. Given the unique position of this lesion, and its capacity to stimulate other nodules in the thyroid, it should be differentiated from other lateral neck masses, such as: thymic cysts, branchial cleft cysts, cystic hygroma, lipomas, lymphadenopathies, cervical teratomas, and lymphomas. In this case, a separate cystic mass was found in the right inferior pole of the thyroid gland and extended to the mediastinum. We confirmed it as TGDC by pathology and histological examination.
Introduction
Thyroglossal duct cyst (TGDC) is the most common congenital mass that arises in the neck. The etiology of TGDC is well known because the embryological development of the thyroid gland is well understood. The primordium of the thyroid gland is located at the base of tongue with a narrow tubular structure called the thyroglossal duct. This connects to the epithelial floor of the mouth by way of the foramen caecum. The thyroid gland extends inferiorly to the midline, and is ventral to the primordium of the hyoid bone. Subsequently, the thyroglossal duct typically disappears during the eighth and tenth weeks of gestation. When the duct does not atrophy, mucosal secretion from the lining epithelium collects and develops a cyst, or abscess formation occurs, resulting in recurring local infection or inflammation.1)
Generally, the TGDC presents as an anterior midline neck swelling that is mobile with deglutition and protrusion of the tongue. A proper diagnosis, in general, includes a careful intake of patient history and a physical examination. It might be difficult to tell whether the swelling is due to metastatic diseases from a primary thyroid cancer or a thyroid goiter in some cases.1) Moreover, TGDC arising from the right inferior pole of the thyroid is extremely rare; and other cystic lesions should be ruled out such as: a simple thyroid cyst, branchial cleft cyst, thymic cyst or parathyroid cyst.2-4) Several cases of intrathyroidal TGDCs were reported in the literature, but there has been no report of one which invaded the mediastinum.2-8) Here, we report a case of TGDC in the inferior pole of the right thyroid and mediastinum that simulated a thyroid goiter. In addition, we review previous related reports of intrathyroid TGDCs.
Case report
A 45-year-old woman presented with a lower neck mass that she had for three years. She had nothing of significance in her past history, nor in her family history, and was asymptomatic except for presentation of a mass in her neck. Physical exam revealed a non-tender, mobile and smooth neck mass about 4× 5 cm in size, in the right inferior pole of the thyroid. There were no other specific findings with either her physical exam, laboratory results, nor any associated cervical lymphadenopathy. The thyroid and parathyroid function tests were in the normal range. Ultrasonography of the nodule revealed a heterogeneous thyroid gland harboring numerous normoechoic focal lesions; and, the nodule (3x6 cm) found on the right lobe, exhibited a low echo and minimal fluid (Fig. 1A). When a needle aspiration of the cystic mass was attempted, only a reddish liquid was visibly drawn. The preoperative CT scan showed a well-defined cystic mass, about 3x7 cm in size, on the lower portion of the right thyroid gland and upper mediastinum (Figs. 1B, 1C). A lack of enlargement of the mass suggests that the lesion is likely cystic. In fact, neck exploration for thyroid and parathyroid was performed under suspicion of thyroid cyst or other adjacent cystic lesion from thymus, parathyroid or metastatic thyroid cancer. A mass was found on the right lower pole of the thyroid gland, 4x5cm in size. The cystic mass was covered by an intact membrane containing a reddish liquid, which adhered to the surrounding gland tissues. The mass was excised from the surrounding tissues. The thyroid gland and the recurrent laryngeal nerve on the right side were both identified and preserved. Subsequent sectioning of the mass revealed a thin-walled cyst storing a large amount of fluid. Representative frozen histologic sections of the cyst wall demonstrated a thin and fibrous wall. Overall, the histopathologic findings were consistent with TGDC; the sections showed pseudostratified ciliated columnar and squamous epithelial lining associated with thyroid follicles in the surrounding stroma (Fig. 2). The findings are comparable to those of a thyroid cyst in pathology. Squamous epithelial cells, on the other hand, are rarely seen in thyroid cysts. This could be the cytologic distinction between a thyroglossal duct cyst and a thyroid cyst.9)
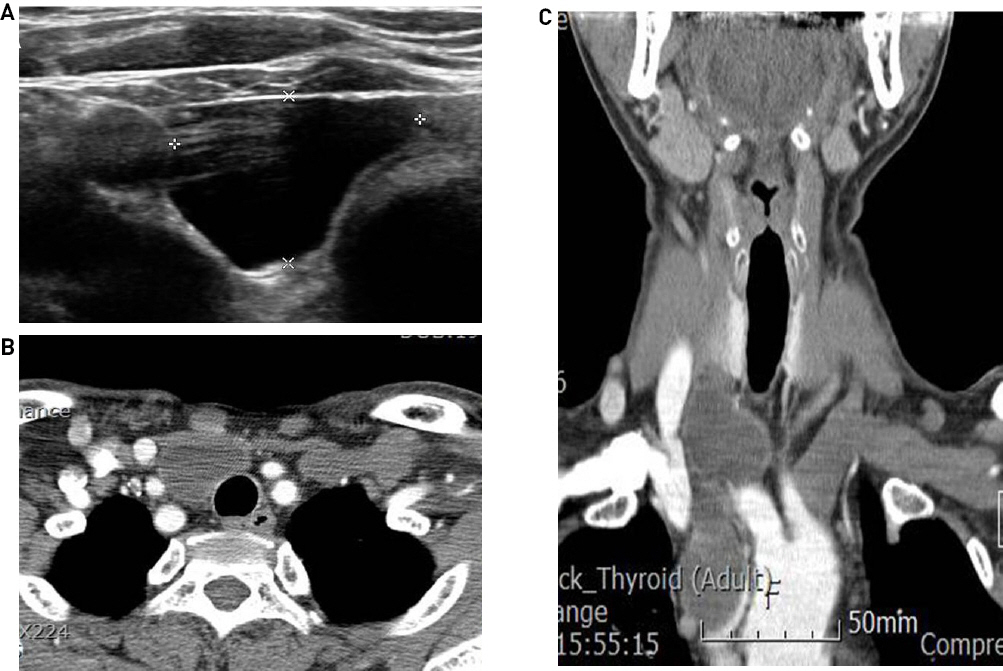
Ultrasonography (A), Axial (B) and Coronal (C) CT images show the cystic mass in the right inferior thyroid pole extending to the upper mediastinum. The cystic mass shows low echo and minimal fluid in right lobe of the thyroid gland, cyst size 3x7cm.
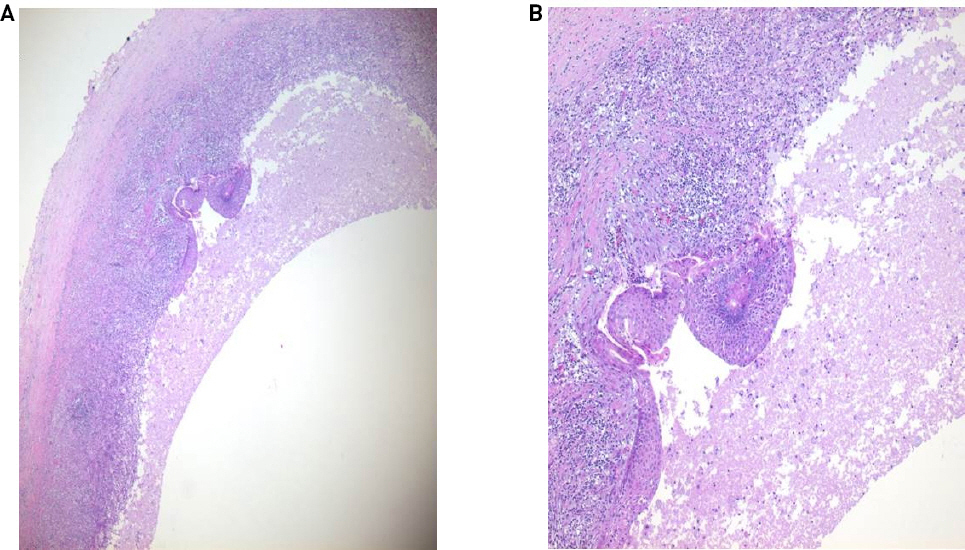
Hematoxylin and eosin (H&E) histology of the thyroglossal duct cyst. Inflamed cystic wall containing necrotic inflammatory exudates in the lumen (x40, A). Squamous epithelium exhibits secondary metaplastic changes, fibrosis and chronic inflammatory cell infiltrates in the cyst wall (x100, B).
The inflamed cystic wall contained necrotic inflammatory exudates in the lumen. The squamous epithelium exhibited secondary metaplastic changes and chronic inflammatory cell infiltrates in the cyst wall. Additionally, the cyst was entirely surrounded by the thyroid tissues. Because there was no visible thyroglossal duct tract, right thyroid lobectomy was done on the patient instead of the sistrunk operation. She was seen in the outpatient clinic and was found to have good wound healing. There were no complications and there has been no recurrence.
Discussion
Thyroglossal duct cysts are the most common congenital neck masses that often occur in pediatric patients; however, at least half are found in the second decade of life and may also present later in adulthood. It is most commonly located at the infrahyoid level.1) However, intrathyroid TGDCs are extremely rare and when found are located on the lateral aspect of the inferior pole of thyroid gland. Accordingly, we should differentiate this cystic mass from other lateral neck masses such as a simple thyroid cyst, branchial cleft cyst, thymic cyst or parathyroid cyst. Specifically, any thyroid tissue found on the lateral aspect of the neck may be suspicious, potentially harboring metastatic thyroid cancer lesions. The brachial cleft cyst (BCC), which is usually found as a second branchial groove cyst and located in the upper lateral neck, develops from the failure of the obliteration of the cervical sinus.2-4) The standard method of differentiation between the two types is via histological examination. The TGDC is made up of non-keratinizing stratified squamous epithelium and respiratory epithelium, whereas the BCC is mostly made up of non-keratinizing stratified squamous epithelium with subepithelial lymphoid tissue4). Parathyroid cysts present mostly as a solitary cystic mass that occur near the lower poles of the thyroid gland or upper mediastinum. They are often misdiagnosed as nodular goiters, cystic degeneration of thyroid gland or even as thyroid carcinoma. When cystic fluid retention or cystic degeneration of a parathyroid adenoma occurs, it is frequently due to an enlargement of microcysts.6) The TGDC carcinoma, which is a papillary carcinoma of thyroid origin, occurs very rarely. The criteria used for the diagnosis of TGDC papillary carcinoma are: 1) The cyst or duct has an epithelial lining with normal thyroid follicles in the cyst wall, as demonstrated by histological identification of TGDC; 2) Close to the tumor, there is normal thyroid tissue; and 3) There is no evidence of primary cancer on histopathologic examination of the thyroid gland.
The treatment of choice for TGDC is the Sistrunk procedure involves removing the mid-portion of the hyoid bone that is continuous with the TGDC. In this case study, the cyst was completely embedded within the thyroid gland and no tract was identified; therefore, a lobectomy was performed. Due to the possibility of metastatic thyroid carcinoma, a diagnostic hemithyroidectomy was strongly recommended in this instance. Thus, the intrathyroid TGDC should be included in the differential diagnosis of lateral neck masses despite its rarity, given that it may be a manifestation of a metastatic carcinoma stimulating the thyroid nodule.5,8) For intrathyroid thyroglossal duct cyst, thyroid resection without the Sistrunk operation was performed in some cases (Table 1). However, there was no recurrence of the cysts after thyroid resection.
In conclusion, intrathyroid TGDC arises from the right inferior pole of the thyroid, is extremely rare, and should be ruled out from other cystic lesions such as: simple thyroid cysts, branchial cleft cysts, thymic cysts, parathyroid cysts, primary TGDC carcinomas and metastatic thyroid carcinomas. Accordingly, its clinical presentation and radiological appearance must be anticipated. Here, we report a very rare case of intrathyroid TGDC in the inferior pole of the right thyroid extending into the mediastinum.
Acknowledgement
This paper was supported by Fund of Biomedical Research Institute of Jeonbuk National University Hospital.
