드물게 발생한 얼굴에 생긴 단일 종괴 형태의 혈관육종에 대한 증례보고
Atypical Angiosarcoma with a Solitary Erythematous Nodule on the Cheek: A Case Report
Article information
Abstract
= Abstract =
Angiosarcoma is a very rare subtype of sarcoma. It mainly occurs in the head and neck, and cutaneous angiosarcoma in this region seems to be a distinctive neoplasm with characteristic clinicopathologic features that differ from those of angiosarcoma in other anatomical locations. The prognosis of angiosarcoma in the head and neck region is poor, and the risk of local recurrence and metastasis is high. We reconstructed an atypical angiosarcoma that presented as a solitary nodule with a shape suggestive of hemangioma on the cheek using a modified bilobed local flap. At a 12-month follow-up visit, the patient in this case showed successful recovery after radiation therapy.
Introduction
Angiosarcoma of the head and neck is a rare type of vascular sarcoma associated with high rates of local recurrence and distant metastasis and a poor prognosis.1,2) Cutaneous angiosarcoma of the head and neck region seems to be a distinctive neoplasm with characteristic clinicopathologic features that differ from those of angiosarcoma in other anatomical locations.1-3) It often presents as multiple purplish-red papules and nodules on the head and neck or the extremities.4) Angiosarcomas of the skin are uncommon, constituting fewer than 1% of all sarcomas and mainly occur in males (sex ratio of 3:1), at an average age ranging from 60 to 80 years.5,6) Cutaneous angiosarcoma primarily occurs in three clinical settings: idiopathic angiosarcoma of the face, scalp, and neck; angiosarcoma associated with chronic lymphedema (Stewart-Treves syndrome); and post-radiation angiosarcoma.6)
We reconstructed an atypical angiosarcoma that presented as a solitary nodule with a shape suggestive of hemangioma on the cheek using a modified bilobed local flap. At a 12-month follow-up visit, the patient showed successful recovery after radiation therapy.
Case report
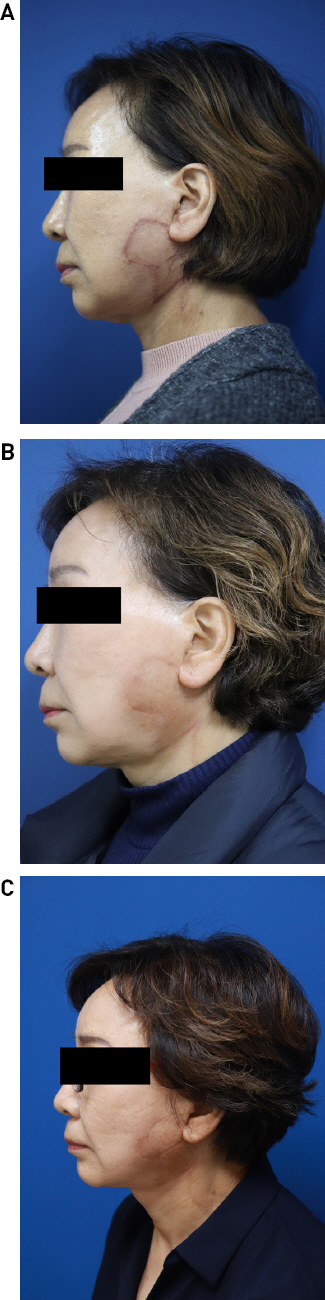
A 69-year-old woman presented to our outpatient clinic with a mass lesion in the form of a solitary nodule with a regular margin on the left lower cheek that had progressed during an approximately 2-month period (Fig. 1A). The mass measured approximately 1.5 × 1.5 cm and presented as a protrusion. The patient had no specific family history or a history of irradiation or lymphedema. We first expected the mass to be a benign hemangioma and performed an excisional biopsy under local anesthesia (Fig. 1B). However, in contrast to our expectations, the histopathological results showed that the mass was an angiosarcoma (FNCLCC grade 2/3) (Fig. 2). When stained with H&E stain, overgrowth of vascular endothelial cells is characteristic, and angiosarcoma can be confirmed by findings of rapid endothelial differentiation when stained with anti-CD31 antibody. Therefore, additional imaging tests were performed before surgery, and PET-CT and face contrast MRI were performed. A reactive lymph node was suspected in the right cervical area and mediastinum, but the possibility of metastasis was low.

Photographs of A 69-years-old woman with solitary mass on left lower cheek. (A) A mass lesion in the form of a solitary nodule with a regular margin on the left lower cheek that had progressed during an approximately 2-month period. (B) Photograph of post-excisional biopsy.
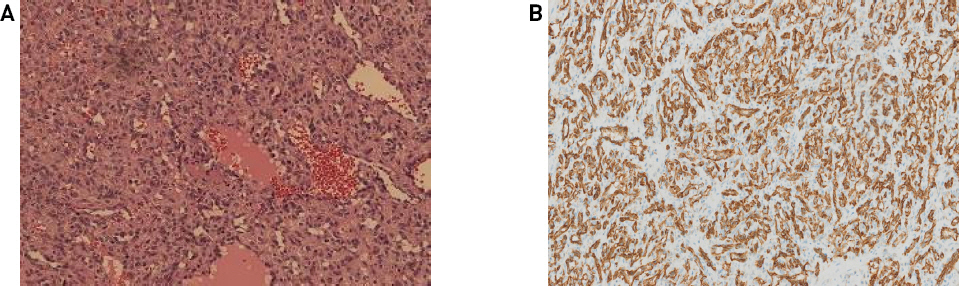
The histopathological image showed angiosarcoma (FNCLCC grade 2/3) (A) H&E stain x 100. (B) Anti-CD31 antibody stain x 400.
A second operation was performed under general anesthesia with wide excision (surgical excision range, 3 cm) and a modified bilobed flap (Fig. 3). An absence of tumor involvement in the margin was verified by frozen biopsy during the operation. Enhanced computed tomography of the neck showed no significant cervical lymphadenopathy and positron emission tomography-computed tomography showed reactive lymph nodes, but these were clinically unrelated. The TNM stage, based on the extent of the tumor (T), the extent of spread to the lymph nodes (N), and the presence of distant metastasis (M) for the cutaneous angiosarcoma, was T1N0M0. We referred the patient to a radiation oncology center for further management and radiation therapy was done starting 3 weeks postoperatively.

Photographs of intraoperative image. (A) This is an illustration of the design for the flap after resection of angiosarcoma. (B) Postoperative photograph after wide excision with a surgical range of 3 cm and a modified bilobed flap.
After radiation therapy, the results of long-term follow-up at 1 month, 6 months, and 12 months postoperatively showed that wound healing was good, and no local recurrence was found (Fig. 4).
Discussion
The types of skin cancer occurring on the face were classified into Basal cell carcinoma, Squamous cell carcinoma, Malignant melanoma, and others (adenocarcinoma, angiosarcoma, extramammary Paget disease, Merkel cell carcinoma, and verrucous carcinoma).12) Cutaneous angiosarcoma is a rare sarcoma of vascular capillary and lymphatic endothelial cell origin with aggressive characteristics, a poor prognosis, and a high risk of recurrence.2,3) Although angiosarcoma can occur anywhere in the body, angiosarcoma in the head and neck region tends to occur on the scalp and face between the ages of 60 and 79.2) It also mainly occurs in males (sex ratio of 3:1) and is a very rare subtype of sarcoma, accounting for fewer than 1% of sarcomas.3-6) Due to its rarity, angiosarcoma is challenging to diagnose, and its differential diagnosis includes intravascular papillary endothelial hyperplasia, Kaposi sarcoma (multiple hemorrhagic sarcoma), Kaposi-like hemangioendothelioma, angio-lymphoid hyperplasia, Kimura’s disease, and amelanotic melanoma.3-11) In many cases, the etiology of angiosarcoma is unknown; however, some important risk factors include prior radiation exposure, chronic lymphedema (Stewart-Treves syndrome), and exposure to carcinogens such as arsenic and vinyl chloride.7-8)
Cutaneous angiosarcoma presents insidiously as an erythematous, violaceous, or bruise-like lesion; these lesions can be nodular, macular, plaque-like, or ulcerative.2,7,8) However, the diagnosis is sometimes delayed because the lesion itself is often confused with rosacea, hemangioma, hematoma, eczema, or infection.3,7,9) Therefore, early clinical suspicion is necessary, and physicians should consider biopsy for skin lesions that resemble angiosarcoma.
Case reports have mainly reported cases of patients with multiple and bullous skin lesions in erythematous maculo-papule forms, or cases where extensive lesion invasion made wide excision difficult, leading to a poor prognosis.3-10) However, our case was an atypical asymptomatic sarcoma, which was easily mistaken for a solitary-nodule hemangioma. It was helpful to perform a biopsy promptly when the patient first presented to our clinic. After the pathological diagnosis, the possibility of remnant cancer can be excluded by wide excision with a surgical margin and by performing frozen biopsy. Although there is no clear guideline for radiation therapy for angiosarcoma, previous studies have demonstrated the effect of radiation therapy on secondary recurrence or prognosis.13) Therefore, in this case, the patient also received radiation therapy. In addition, attention should be paid to when dissecting the facial nerve branch, as it exists more deeply than the sub-superficial musculoaponeurotic system (SMAS), so it is necessary to understand the anatomy of the above structure during surgery and dissect it. Given the possibility of an initial misdiagnosis, it is important to perform a histological biopsy without excluding the possibility of malignancy. In addition, for lesions diagnosed as angiosarcoma, wide excision and appropriate radiation therapy should be performed as soon as possible to prevent local recurrence and to achieve a favorable prognosis. There is no guideline for elective neck dissection for head and neck angiosarcoma yet. It is expected that a good prognosis and outcomes without sequelae will be possible in the future through an agreement on the exact scope of resection and treatment method according to staging.