Introduction
Squamous cell carcinoma is the most common lip-related malignancy with 90% of the cases involving the lower lip.1) The treatment of squamous cell carcinoma of the lips depend on the size and location, but is usually surgically excised completely with possible postoperative radiation therapy for advanced lesions.2) Oncologic wide excision of these lesions often results in large lip defects and reconstruction with good functional and aesthetic outcome is the biggest challenge for surgeons. Several techniques have been described for lower lip reconstruction depending on the defect’s size and location. Defects that affect less than one-third of the lower lip length are usually treated with primary closure, but larger defects that affect more than two-thirds of the lower lip need more complex techniques.3) The Karapandzic flap is one of the useful large defect reconstruction techniques of the lower lip using neurovascular myocutaneous flaps based on labial arteries first described by Karapandzic in 1974.4) This flap’s advantage is that neurovascular bundles are identified and preserved during dissection; hence, there is lip sensory and motor function preservation. Additionally, it is a one-stage reconstructive procedure. This flap’s disadvantages are that the lip circumference is reduced, which can cause microstomia.5,6) However, it can be corrected with comissuroplasty in a second surgery if there is postoperative microstomia.7) This paper aimed to report a case of large lower lip defect reconstruction using the Karapandzic flap with a commissuroplasty carried out in a second operation.
Case Report
An 86-year-old female patient with a history of hypertension, colorectal cancer, and dysliplidemia presented our hospital with complaints of a rapidly growing mass involving her lower lip for the last 3 months. A punch biopsy was performed at another hospital and the patient was diagnosed with moderately differentiated squamous cell carcinoma. On clinical examination, approximately 5 × 2.5 × 1.5 cm raised intraoral and cutaneous area, multiple fungating, ulcerated mass extending from the left commissure up to the lower lip midline which affected two-third of the lower lip (Fig. 1). Magnetic resonance imaging and torso PET-CT showed enlarged lymph nodes in both neck Level IA and left Level IB with no distant metastasis evidence (cT4aN2cM0). Surgical excision and lower lip reconstruction with modified radical neck dissection were planned. A hockey stick incision was made at the left neck area and level I, II, and III modified radical neck dissection was performed. The lower lip tumor wide excision was performed with a 10-mm safety margin under the general anesthesia. Frozen biopy confirmed squamous cell carcinoma with tumor-free margins (Fig. 2A). After surgical resection of the tumor, the lower lip defect measured about 6 × 2.5 cm which was over two-third of the total lip width (Fig. 2B). The lower lip defect was reconstructed with bilateral Karapandzic flap. The incisions were made horizontally along the lower border defect extending to the bilateral oral commissures and nasolabial folds. During the dissection, the neurovascular bundle was identified and preserved. The contralateral flap was made longer in order to allow greater mobility and bilateral flaps were medially rotated and advanced for closure (Fig. 2C). Microscopic findings demonstrated abundant eosinophilic cytoplasm, atypical keratinization, and squamous epithelial cells arising from the epidermis and extending into the dermis consistent with a moderately differentiated squamous cell carcinoma. Postoperatively, the patient presented with relatively good oral muscular and sensory function, but had microstomia with a 19-mm interridge distance and a 21-mm intercommissural width. (Fig. 3). The secondary commissuroplasty was performed 4 weeks postoperatively. The triangular excision lines were designed along bilateral mouth corners (Fig. 4A). Full thickness incisions were made exposing the buccal mucosa and orbicularis oris muscle. The buccal mucosa, labial mucosa and orbicularis oris muscle of the blunted commissure were divided horizontally extending to the planned commissure’s apex. The buccal mucosa was advanced laterally, superiorly and inferiorly to form the new vermilion border. Intraoperative photographs showing the mouth webbing had disappeared, the interridge distance was increased from 19 mm to 25 mm and the intercommissural distance was increased from 21 mm to 45mm (Fig. 4B). At 4 months after secondary commissuroplasty, the patient was satisfied with the lip morphology and function (Fig. 5).
Fig. 2
(A) Intraoperative photographs. Incision design of 10-mm safety margin and bilateral Karapandzic flaps. (B) Large defect affects more than two-thirds of the lower lip after wide excision. (C) The bilateral flaps were raised and medially rotated for closure.
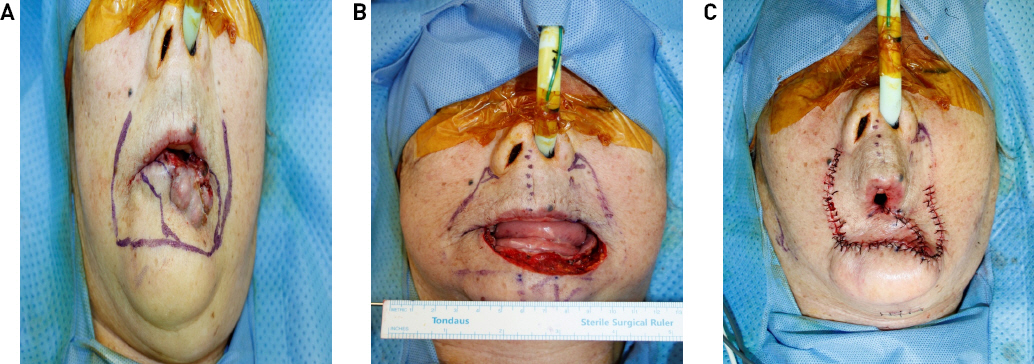
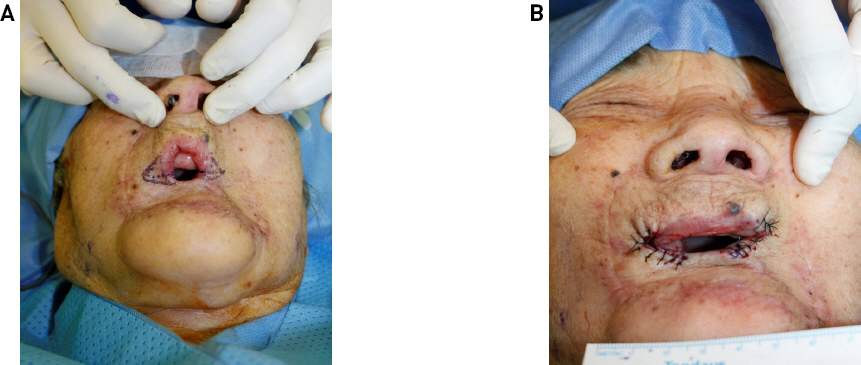
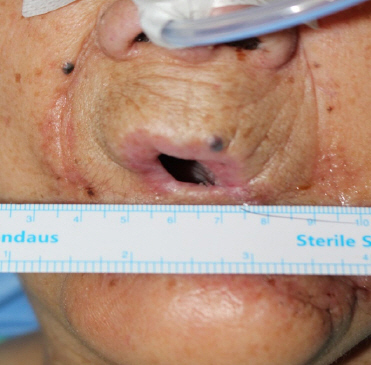
Fig. 3
At 2 weeks postoperatively showing microstomia with a 19-mm interridge distance and 21-mm intercommissural width.
Disussion
Lip cancer is a common malignancy accounting for approximately 30% of oral cavity malignant tumors.8) The most frequent malignancy related to the lips is squamous cell carcinoma and 90% of cases involved in the lower lip.1) Oncologic wide excision with safety margins plays an important role in lip malignancy treatment and large defects are often encountered.9) Several reconstructive techniques have been described depending on the defect’s size and location. For small defects affecting less than one-third of the lip, it can be treated by primary closure or advancement flap.10) Larger defects require local or distant flaps use. There are various techniques for reconstruction including Karapandzic flap, Abbe flap, Estlander flap, Bernard-Burrow flap, Gilles fan flap or combinations.9,11) In 1974, Karapandzic introduced the technique to repair large lip defects using neurovascular myocutaneous flaps based on the superior and inferior arteries. This technique is a Gillies fan flap modification, which often results in oral incompetence due to lip denervation.4) In this modification, the key lip neurovascular bundles are kept intact, thus preserving lip sensation, motor function and optimizing tissue vascularity.12) This is a sensate axial musculomucocutaneous flap and is useful for closing one-half to two-thirds upper lip defects or up to three-quarters lower lip defects.6) In the preoperative design, it is helpful to mark the patient’s nasolabial, labiomandibular, and mental creases. These creases are easily seen in older patients, but is sometimes not obvious in younger patients. In such cases, patients should be asked to smile to exhibit the creases. Semicircular incision lines should be drawn from the defect toward the nasolabial creases bilaterally. The skin incisions are made along the designed line followed by careful dissection to identify the labial arteries and nerve branches. The orbicuralis oris muscle is identified and separated carefully from adjacent tissues while preserving the lip elevator and depressor muscles, such as the levator labii superioris, levator anguli oris, and depressor anguli oris. However, these muscles could be released to achieve sufficient flap mobility in larger defects. The other major advantages of the Karapandzic flap are that it is a single-stage surgical procedure and its quick execution once learned.5) As every surgery technique has its pros and cons, the Karapandzic technique’s major drawback is that the lip circumference is reduced, can cause microstomia, and loss of the commissures.4,6) Microstomia results in not only adverse cosmetic problems, but also functional impairments, such as pronunciation, difficulty with food intake, and poor oral hygiene.13) In approximately 24% of patients who underwent the Karapandzic flap for lip reconstruction, secondary commissuroplasty procedures were required to correct microstomia.4) Commissuroplasty methods are abundant and range from simple advancement flap to complex reconstruction using free flap. In our case, buccal mucosal advancement flap technique, which is the simplest method for commissuroplasty, was used. The procedure produced an acceptable aesthetic and functional result. In summary, the Karapandzic flap is one of the useful techniques for large lip defect reconstruction. This technique is a single-stage procedure and allows important neurovascular bundle preservation, thus resulting in lip sensory and motor function preservation. The major disadvantage of this technique is microstomia, but this can be easily corrected with secondary commissuroplasty. For large lip defect corrections, the Karapandzic flap is a good option with satisfactory functional and aesthetic results. However, there are some limitations concering lip functions, such as oral competence, speech, and social expression. Further study is needed for a complex set of motions between the circular contraction of the orbicularis oris and the radial action of the lip elevators and depressors.