내경정맥의 변형을 유발한 거대 경부 지방종
Giant Lipoma in the Lateral Neck Causing Internal Jugular Vein Deformity
Article information
Abstract
= Abstract =
Lipoma is one of the most common benign soft tissue tumors. However, giant lipomas compressing and deforming the neurovascular structure rarely occur in the lateral neck. A 70-year-old man visited our outpatient clinic for treatment of a visible painless neck mass that had been identified 2 years prior. Neck magnetic resonance imaging revealed that a 10 × 9 × 4 cm fatty mass located between the sternocleidomastoid and sternohyoid muscles invaded the carotid sheath. Under general anesthesia, the mass was excised without damage to the adjacent neurovascular structures. Upon histopathological examination, the mass was identified as a lipoma. During the surgery, enlargement of the internal jugular vein was observed under the resected mass. However, on ultrasound examination, the function of the internal jugular vein was evaluated as good. No recurrence or neurological and vascular complications were reported during a 6-month follow-up after the surgery. As a giant lipoma located in the deep layer of the lateral neck can deform important cervical structures, its impact on the surrounding structures should be carefully assessed preoperatively to minimize the rate of possible complications.
Introduction
Lipoma is one of the most common benign tumors which can occur in any fat tissue of the body.1,2) Approximately 13% of lipomas occur in the head and the neck, usually presenting in the posterior neck.3) A lipoma larger than 10 cm in any dimension or than 1000 g in weight is referred to as a ‘giant lipoma’, and this type of lipoma is rare in the lateral neck.4)
The neck contains the crucial blood vessels and nerves. Tumors in the neck are clinically important because they can cause significant complications, including cosmetic problems, voice changes, and impaired swallowing functions.5) However, a giant lipoma that might compress and deform the neurovascular structures is rare in the lateral neck. To date, there has been one reported case of aneurysmal change in the internal jugular vein due to a myxoid lipoma in the neck.6)
Here, we report a rare case of giant lipoma located in the lateral neck and causing internal jugular vein deformity.
Case report
A 70-year-old man visited our outpatient clinic for the treatment of a visible painless neck mass that had been identified 2 years prior (Fig. 1). No neurological symptoms, such as dyspnea, dysphagia, and hoarseness, were observed. The patient’s chronic diseases, including hypertension, diabetes, and chronic kidney disease, were effectively managed.
Neck magnetic resonance imaging (MRI) revealed that a 10 × 9 × 4 cm fatty mass between the sternocleidomastoid and sternohyoid muscles invaded the carotid sheath (Fig. 2). The large fatty mass caused the trachea to shift its midline to the right and pressed the lumen of the left internal jugular vein (Fig. 2).
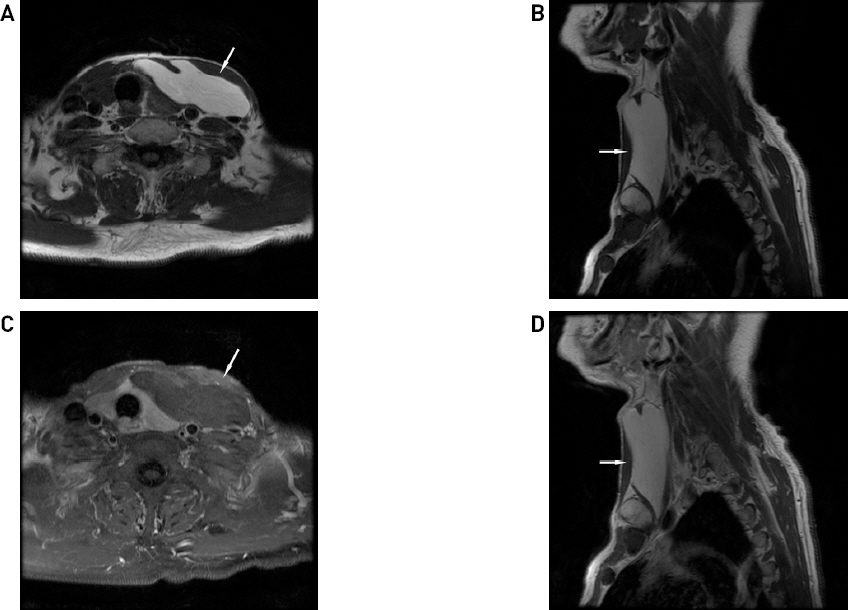
Preoperative neck MRI showing a 10 × 9 × 4 cm fatty mass (white arrows) between the sternocleidomastoid and sternohyoid muscles. (A) Axial T1-weighted image (non-enhanced). (B) Sagittal T1-weighted image (non-enhanced). (C) Axial T1-weighted image (enhanced). (D) Sagittal T1-weighted image (enhanced).
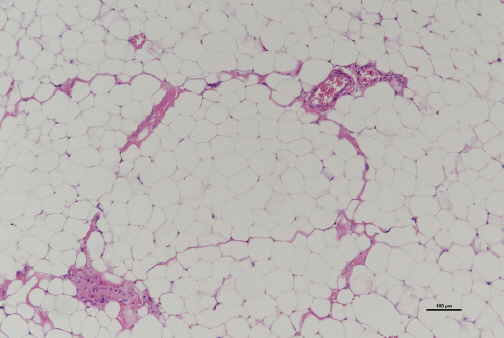
Under general anesthesia, the mass was excised without damage to the adjacent neurovascular structures, and enlargement of the internal jugular vein was observed under the resected mass (Fig. 3). The surgical wound healed without any complications. Histopathological examination identified the mass as a lipoma (Fig. 4). On ultrasound (US), the function of the internal jugular vein was evaluated as good. No recurrence or neurological and vascular complications were reported during a 6-month follow-up after the surgery.
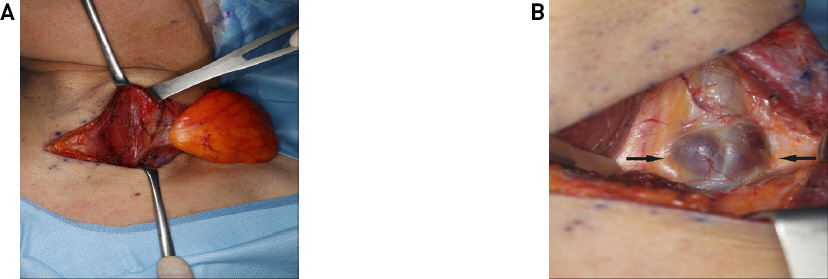
Intraoperative photographs. (A) A large yellowish mass dissected under the sternocleidomastoid muscle. (B) Enlargement of the internal jugular vein following mass excision (black arrows).
Discussion
Lipoma, a soft tissue tumor of mesenchymal origin, is the most common benign tumor in the elderly.7) Lipomas can be subcutaneous, subfascial, intermuscular, etc, depending on where it occurs.4) Lipoma most frequently occurs in the subcutaneous layers, and the incidence of intermuscular lipomas is rather low, i.e. 0.3% to 1.9%.8) In this case, a giant lipoma in the intermuscular layer of the lateral neck compressed on the surrounding structures. Of note, giant lipoma must be distinguished from liposarcoma with metastatic potential.3)
Similar to diagnosing other soft tissue tumors, imaging methods such as US, computed tomography (CT), and MRI are used to diagnose lipomas. US is used for initial studies because it is a non-invasive and inexpensive method.7) CT scans reveal a lipoma as a homogenous, low-density lesion with clear boundaries. MRI scans provide a clear view of the boundaries between a lipoma and its surrounding structures and help to distinguish lipomas from malignant tumors, such as liposarcomas. Fine-needle aspiration biopsy might be considered when imaging studies do not provide clear results.2) In this case, neck MRI revealed that a giant lipoma caused a split of the common carotid artery and internal jugular vein by invading the carotid sheath. In addition, it showed that the giant lipoma caused the trachea to shift its midline to the right and pressed the lumen of the left internal jugular vein. Although the size of the mass was large, needle biopsy was not performed because there were no findings suggestive of malignancy.
The treatment of choice for lipoma involves a complete surgical excision, with a low recurrence rate of 1%-2%. Liposuction, another treatment option for lipoma, has the advantage of reducing associated incision scars. However, it is challenging to completely remove a giant lipoma by liposuction, and the approach is associated with a high recurrence rate.9) In this case, complete surgical excision of the giant lipoma was performed because the possibility that it was a malignant tumor could not be completely ruled out.
The neck is an important part of the body, as it connects the head and chest and contains critical and complex neurovascular structures.5) Large masses, which occur in deep layers of the neck, might cause symptoms, such as dyspnea, dysphagia, and hoarseness, by compressing the airways, esophagus, and neurovascular structures.10) Surgical removal of tumors from the neck should be performed carefully to prevent functional complications of breathing, deglutition, and vocalization.11) In this case, no functional problems related to the neck were observed in the patient before and after surgery, but the giant lipoma in the lateral neck caused the deformation of the internal jugular vein. No damage to the vessel wall of the internal jugular vein occurred during surgery, but the enlargement of the vessel wall was observed under the resected mass.
The cause of internal jugular vein aneurysm is unknown; however, several related hypotheses have been reported in previous studies. Pathological studies have shown that the loss of elastic layers, hypertrophy of the connective tissue, and local intimal thickening might be the causes of jugular vein aneurysm.12) Thus, innate structural defects in the venous wall might be an important factor in the occurrence of this pathology. Other contributing factors include mechanical compression or trauma to the vein and defects of the venous valve at the bifurcation site of the internal jugular vein and the external jugular vein. The conditions that might obstruct the jugular vein, such as thoracic outlet syndrome or anterior scalenus compression and that might increase intrathoracic pressure chronically, are also important factors related to the development of jugular vein aneurysm.12) In this case, there was no evidence of distal jugular venous obstruction. Tawil et al. reported a case of a large myxoid lipoma encasing a collapsed aneurysmal jugular vein.6) Similarly, in our case, continuous mechanical compression by giant lipoma is suspected to have deformed the vessel walls of the internal jugular vein.
In summary, as a giant lipoma located in the deep layer of the lateral neck can cause deformities of important cervical structures, a thorough preoperative assessment regarding its relationship with the surrounding structures is necessary to minimize the rate of possible complications.
Notes
Ethical approval
The study was approved by the Institutional Review Board of Chonnam National University Hospital (CNUH-EXP- 2021-099) and performed in accordance with the principles of the Declaration of Helsinki.
Patient consent
The patient provided written informed consent for the publication and the use of his images.