Case report
A 73-year-old woman was diagnosed with recurrent sebaceous carcinoma of the nose. She had developed basal cell carcinoma of the nose 12 years ago and had a history of two recurrences despite treatment. Sebaceous carcinoma of the right upper lip was treated by wide excision and reconstruction with a left radial forearm chimeric flap 3 years ago. In the same year, an additional wide excision and reconstruction was performed with a local flap for a recurrence in the premaxilla.
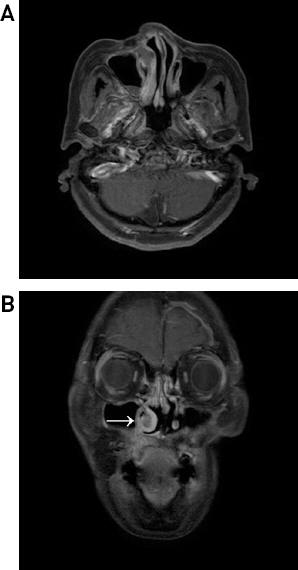
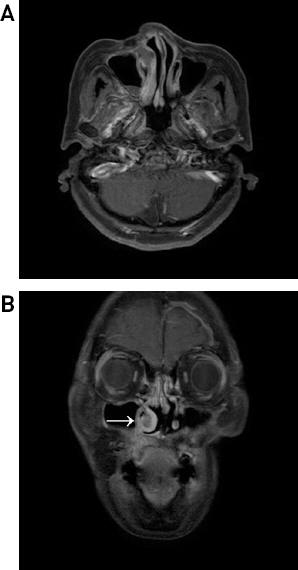
On the present visit, an MRI revealed a 1.5-cm soft-tissue lesion at the anterior portion of the inferior turbinate on the right side. Subsequently, wide excision and reconstruction were planned for suspected recurrence (Figs.
1A and
1B). Wide excision, including the right cheek, nose, upper lip, maxilla, and columella, was performed with negative frozen biopsy results (
Fig. 2A). Three-dimensional flap reconstruction was planned for the coverage of the subsequent Brown type II subtotal maxillary defect. The right free radial forearm flap was divided into three parts and designed so that all of the nasal, oral, and external facial areas could be filled. The flap was harvested in an elliptical shape, and the premaxilla skin, oral mucosal side, and nasal mucosal side were made starting from the side closest to the pedicle. At this time, the skin defect on the right cheek and the oral lining defect on the palate were covered with the flap skin that was maintained, and the nasal mucosal side was inset after de-epithelization. The proximal and distal ends of the pedicle of the radial forearm flap were explored to acquire sufficient length. The proximal end of the radial artery and vein were anastomosed end-to-end to the right facial artery and vein. Since the columella is a separate subunit, we also harvested the right preauricular flap, positioned it into the columellar deficit, and anastomosed it to the distal portion of the pedicle of the radial forearm flap in an end-to-end fashion (Figs.
2B,
2C, and
2D).
Fig.┬Ā1
Magnetic resonance images (T1 weighted) show a new soft-tissue lesion approximately 1.5 cm with restricted diffusion in the right inferior turbinate anterior portion (arrow). (A) Preoperative axial view. (B) Preoperative coronal view.
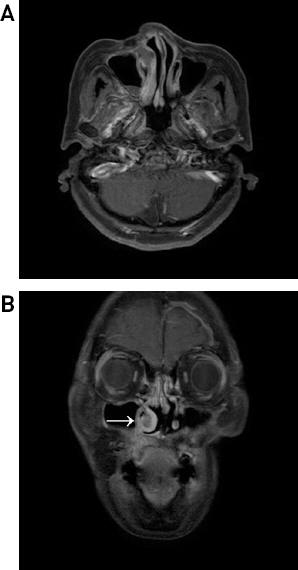
Fig.┬Ā2
Intraoperative photographs and schematic diagram of the surgery. (A) Brown type II defect after subtotal maxillectomy. The maxillary arch, palate, anterior, and lateral walls were excised while preserving the orbital floor. (B, C) Immediately after reconstruction using radial forearm and preauricular double free flaps. Reconstruction was achieved using radial forearm and preauricular double free flaps with a pedicle connection. Nasal tubes were used to prevent airway blockage. (D) Schematic diagram of the surgery. The schematic diagram shows the pedicles and reconstruction sites of the radial forearm and preauricular flaps. The radial forearm flap was divided into three parts, and the premaxilla skin, oral mucosal side, and nasal mucosal side were made starting from the side closest to the pedicle. The skin defect on the right cheek and the oral lining defect on the palate were covered with the flap skin that was maintained, and the nasal mucosal side was inset after de-epithelization. The radial forearm flap was anastomosed to the facial artery and vein, whereas the preauricular flap was anastomosed with the distal portion of the radial forearm flap pedicle in an end-to-end fashion. J/P, Jackson Pratt drain.

Nasal tubes were inserted into the nostrils to prevent airway blockage. The oro-sinonasal communication was effectively separated, allowing good pronounciation and a patent airway (Figs.
3A and
3B). There were no signs of infection after surgery. The two flaps remained viable, and the patient recovered uneventfully. Therefore, we considered that the radial forearm and preauricular double free flaps with the pedicle connection method was effective in this specific case.
Fig.┬Ā3
Three-month postoperative photographs. The double free flap was successfully engrafted without complications. The oro-sinonasal communication was effectively separated, allowing good pronunciation and a patent airway. There were no signs of infection after surgery. (A) Frontal view. (B) WormŌĆÖs-eye view.

Discussion
Subtotal maxillectomy defects with columella deficit are challenging to reconstruct due to their three-dimensional nature, involving the maxilla and mucosal lining, nasal airway, and soft tissue.
1) The maxilla separates the oral and nasal cavity and forms a bony framework. In addition to the functional role, the maxilla is aesthetically vital due to its location covering the center of the face, which affects the facial contour, making it a major factor for reconstruction. Brown classification is widely used to classify the maxillary defects.
2) For post-maxillectomy defects, the types are classified according to whether the main structures are preserved, and an effective reconstruction method is chosen accordingly.
In the present case, the patient underwent a low unilateral alveolar maxillectomy, and the defect was classified as Brown type II. Type II maxillectomy means the removal of the maxillary arch, palate, anterior, and lateral walls while the orbital floor is preserved.
3) Since this patient had a unilateral type II defect, the separation of oro-sinonasal communication was key to reconstruction.
4) Therefore, each free flap had to be designed to compensate for the skin defects and separate the oral cavity and nasal cavity.
5) Instead of using artificial bones and titanium mesh to support the patientŌĆÖs midface framework, we chose a radial forearm flap that was effectively used to reconstruct three-dimensional structures, including mucosal layers.
6) The oral cavity and nasal cavity were effectively separated with the free radial forearm flap which was designed three-dimensionally. Furthermore, the surface of the maxillary defect was reconstructed aesthetically.
Reconstruction using an osteocutaneous flap was also considered. However, the maxillary defect was small, and the patient wanted minimal donor morbidity. Therefore, reconstruction was performed only using fasciocutaneous flaps.
7) This allowed for rapid reconstruction with minor donor site complications. However, the soft tissue seemed somewhat inadequate after the operation, and applying dental prosthetics and implants in the future may become challenging. Using a myocutaneous flap, such as the anterolateral thigh flap, would have provided a larger amount of soft tissue to prevent postoperative depression.
8) However, myocutaneous flaps are bulky, cannot be easily organized into the desired shape, and may require revisional operations. Osteocutaneous flaps are not only effective for structural support but also for maintaining contour and allowing a straightforward application of dental prostheses and implants in the future. However, using an osteocutaneous flap prolongs the operation time and increases donor site morbidity. Their use also results in relatively unreliable skin paddle and increased risk of flap necrosis.
9,
10) In Class IIa defects, prevention of oro-sinonasal communication is the most critical issue, and reconstruction using fasciocutaneous flaps can help achieve the intended purpose.
The nose is a functional unit located in the center of the face and consists of topographic subunits, such as the nasal tip, dorsum, and alar lobules. When a significant defect appears in these subunits, it is practical to repair them as a whole subunit rather than partially.
11) If proper reconstruction is performed for each subunit, there is an aesthetic advantage, i.e., the postoperative scar and contracture can simulate the shadow and curvature of normal tissue, respectively. Therefore, it is necessary to consider the subunit principle for the practical and aesthetic reconstruction of the nasal subunit.
11,
12) Considering these reasons, we decided to use a separate free flap for the columella nasal subunit during maxillary reconstruction. The preauricular free flap was selected to reconstruct the nasal subunit. The preauricular flap is a thin flap with the superficial temporal artery and vein as the pedicle, and has the advantages of having a consistent anatomy and long pedicle, being relatively easy to harvest, and resulting in low donor morbidity. Although it is difficult to take a large skin paddle, it is the facial skin itself and can be elevated with a chondrocutaneous flap, so it can be effectively used for the reconstruction of the face, especially the nose, where the defective area and volume are not large. Since it has a proper color, matching texture, and sufficient blood supply, it is used for columella lengthening and reconstructions of the various nasal subunit.
13)
Final reconstruction was performed by adequately designing the preauricular flap and connecting it to the distal end of the pedicle of the radial forearm flap. The use of a double free flap for reconstruction requires accessible recipient vessels with appropriate diameters. The radial forearm flap is advantageous because the distal end can be used as a recipient vessel with a long pedicle. Reconstruction using the double free flap was possible by properly designing each flap three-dimensionally and connecting them effectively. Thus, the radial forearm flap and preauricular flap are excellent combinations for the functional and cosmetic reconstruction of maxillary defects. The use of double free flap for this type of reconstruction and anastomosis of the other free flap to the distal part of the pedicle of one flap is novel and effective. In similar reconstructions, more favorable cosmetic outcomes can be expected through additional experience using two free flaps. Further reconstruction will be considered if the contracture is worsened by radiation therapy or if the patient desires cosmetic improvement. At present, correction of the right alar base and nostril is required. Composite chondrocutaneous graft transfers or paranasal myocutaneous flap grafting, and Z-plasty combined with a local flap can be performed to reconstruct the alar base and used to improve the shape of the nostril.
14,
15)
In conclusion, a post-maxillectomy Brown type II defect was reconstructed using radial forearm and preauricular double free flaps. This allowed effective separation of the oro-sinonasal communication caused by the defect. Moreover, the airway was functionally maintained, and the nasal subunit was aesthetically reconstructed.