갑상선암 표적치료의 최신지견
What’s New in Molecular Targeted Therapies for Thyroid Cancer?
Article information
Abstract
= Abstract =
Thyroid cancer refers to various cancers arising from thyroid gland. Differentiated thyroid cancers (DTCs) include papillary, follicular, and Hurthle cell carcinomas and represent cancers retain normal thyroid functions such as iodine uptake. Radioactive iodine (RAI) is generally used for upfront treatment of metastatic DTCs, but RAI refractory DTCs remain to be clinical challenges. Sorafenib and lenvatinib were approved for the treatment of RAI refractory DTCs and more recently, genomics-based targeted therapies have been developed for NTRK and RET gene fusion-positive DTCs. Poorly differentiated and anaplastic thyroid cancers (ATCs) are extremely challenging diseases with aggressive courses. BRAF/MEK inhibition has been proven to be highly effective in BRAF V600E mutation-positive ATCs and immune checkpoint inhibitors have shown promising activities. Medullary thyroid cancers, which arise from parafollicular cells of thyroid, represent a unique subset of thyroid cancer and mainly driven by RET mutation. In addition to vandetanib and cabozantinib, highly specific RET inhibitors such as selpercatinib and pralsetinib have demonstrated impressive activity and are in clinical use.
Introduction
The incidence of thyroid cancer increased dramatically over time from 3.6 per 100,000 in 1973 to 8.7 per 100,000 in 2002, a 2.4-fold increase in the United States.1) Although most of the increase are attributed to increase in small papillary thyroid cancers associated with increased detection, incidence of stage IV thyroid cancer has also increased from 2000 to 2013.2) While prognosis of differentiated thyroid cancers (DTCs) such as papillary, follicular, and Hurthle cell cancers is relatively favorable, management of more aggressive types of thyroid cancers such as medullary, poorly differentiated, and anaplastic carcinomas remain to be challenging. Majority of thyroid cancers are diagnosed in early stage and can be treated surgically, although patients with more advanced disease require multidisciplinary care involving endocrinologist, radiation oncologist, and medical oncologist. Traditionally, systemic therapy has played limited roles in care of thyroid cancers, mainly for patients with anaplastic thyroid cancers (ATCs) and poorly differentiated thyroid cancers (PDTCs). However, recent advances in genomics research opened an era of targeted therapy and transformed the treatment of advanced thyroid cancers with approval of multiple targeted therapy agents for radioactive iodine refractory DTCs, medullary thyroid cancers (MTCs), and selected PDTC/ATC patients. In this review, we will go over biology of thyroid cancers, current landscape of available targeted therapy and emerging targeted therapy.
Biology of thyroid cancers
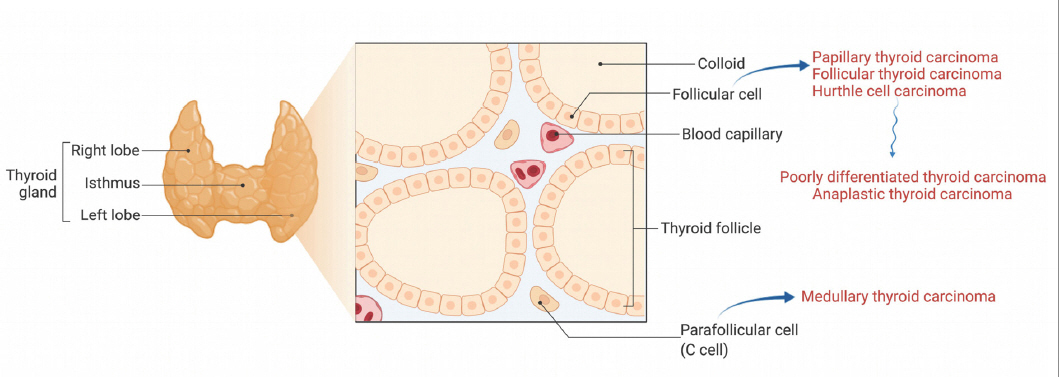
Histologically, thyroid gland is consisted of follicular cells and parafollicular cells. Follicular cells form thyroid follicles which serve as functioning units of thyroid gland and produce thyroid hormones (Fig. 1). Parafollicular cells, also known as C cells, perform a supporting role and produce calcitonin. Most thyroid cancers arise from follicular cells and more differentiated forms such as papillary thyroid cancers (PTCs) and follicular thyroid cancers (FTCs) frequently retain expression of sodium iodine transporter (NIS) and uptake iodine. Less differentiated cancers from follicular cells (PDTC and ATC) can result from transformation of DTCs or can present as de novo disease.3) MTCs represent unique subset of thyroid cancer and arises from parafollicular cells. MTCs do not express NIS and do not uptake iodine. MTCs can present as part of a familial cancer syndrome resulting from germline mutations in RET.
Differentiated thyroid cancers
DTCs account for majority of thyroid cancers, and PTCs are the most common subtype among DTCs. Radioactive iodine (RAI) is highly active treatment for DTCs and relies on thyroid cancer cell’s functioning NIS expression. De-differentiation of cells as result of MAPK pathway activation can lead to NIS repression and RAI refractoriness. Exploration of genomic landscape of papillary thyroid cancers by The Cancer Genome Atlas (TCGA) Research Network revealed that BRAF V600E mutated PTC, which had the strongest activation of the MAPK pathway, also had the most de-differentiated state with low expression of SCLC5A5 which encodes NIS.4) This finding opened a possibility of re-differentiation therapy with agents targeting MAPK pathway to restore NIS expression and iodine uptake. In an animal model with inducible expression of BRAF V600E mutant in thyrocytes, investigators discovered that turning off BRAF V600E expression restores thyroid follicular architecture, thyroid specific gene expression and RAI uptake.5)
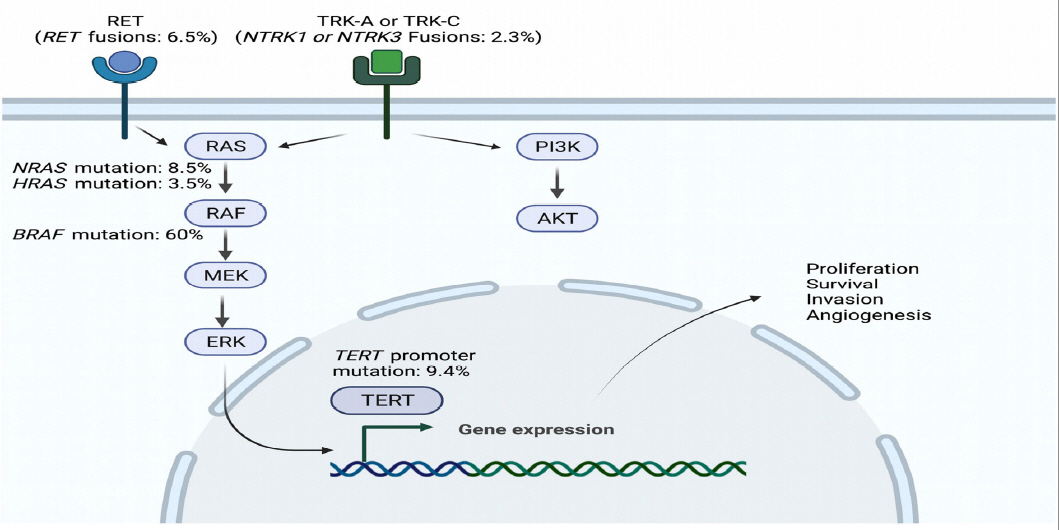
Comprehensive genomic analysis of 496 PTCs in TCGA project revealed frequent mutations in BRAF (60%), TERT promoter (9.4%), NRAS (8.5%) and HRAS (3.5%) as well as gene fusions of RET (6.5%), BRAF (2.3%), NTRK1 and NTRK3 (2.3%). (Fig. 2) These genomic alterations have been well described in various human cancers and are known to promote proliferation, survival, invasion, and angiogenesis. However, besides TERT promoter mutation, other alterations are in a oncogene which can be targeted with various small molecules. It is interesting to note that mutations in PI3K/AKT pathway (PIK3CA 6%, PTEN 2%) and tumor suppressor genes such as TP53 (10%), MEN1 (3%), NF1 (2%) and NF2 (2%) are found more frequently in a cohort of PTC patients with more advanced disease.6) FTCs exhibited distinct profile with frequent RAS gene mutations (NRAS 43%, HRAS 18%, KRAS 5%) and TERT promoter mutations (71%). However, BRAF mutation was rare in FTC. Hurthle cell carcinoma also revealed to harbor unique genomic profile with few BRAF or RAS mutations, but relatively common TP53 mutations (up to 20%).6,7)
In PTC, presence of BRAF V600E mutation has been associated with worse overall mortality in large multicenter retrospective studies.8,9) Furthermore, presence of both BRAF V600E and TERT promoter mutation turned out to be associated with the worse recurrence free survival, compared to patients who has either of those mutations.9) While these findings are intriguing, it has not been validated in a prospective setting yet.
Poorly differentiated thyroid cancers/Anaplastic thyroid cancers
PDTC and ATC represents a rare subset of thyroid cancer patients and account for less than 5% of thyroid cancer patients. The most frequently mutated gene in ATC is TP53 and TERT which is observed in 65% of ATC patients. Approximately 41% of ATC patients harbored BRAF mutation and 27% had RAS mutations. Alterations in cell-cycle genes such as CDKN2A and CDKN2B (copy number loss or loss-of-function mutations) and CCNE1 (copy number gains) were also found in 29% of ATC patients.6) PDTC exhibited less frequent mutations in TP53 and other tumor suppressor genes with similar rates of BRAF and RAS mutations. However, PDTC tended to have similar rates of TERT promoter mutations and slightly more frequent mutations in PI3K/AKT pathway.10)
Medullary thyroid cancers
MTC accounts for 3-5% of all thyroid cancers and the vast majority retain ability to secret calcitonin. Calcitonin is secreted by both normal and neoplastic thyroid C cells and it is a highly sensitive and specific tumor marker for MTC. Its level can reflect disease burden and was shown to correlated with initial tumor staging.11) Carcinoembryonic antigen (CEA) is only produced by neoplastic thyroid C cells and higher level of CEA is also known to be predictive of a poor outcome with rapidly progressing disease.12) Calcitonin has a short half-life of 30 hours and more rapid decline is observed with treatment response. CEA has a longer half-life of 5 days and can take longer to respond.13)
About 25% of MTCs can occur as a part of hereditary cancer syndrome, Multiple Endocrine Neoplasia (MEN) 2A and MEN 2B, caused by a germline activating mutation in the RET (rearranged during transfection) proto-oncogene.14) About 75% of MTCs are present in sporadic form and a somatic mutation in RET is observed in up to 50% of the sporadic cases.15) The rest of sporadic MTC cases are known to harbor HRAS or KRAS mutations - indeed, approximately 90% of MTCs have mutually exclusive mutations in RET, HRAS and KRAS.16) Gene rearrangements of ALK and RET have been recently described in sporadic MTC,17,18) adding complexity to the biology.
Established targeted therapy for thyroid cancers
Differentiated thyroid cancers
DTC is considered RAI refractory when there is no radioactive iodine uptake in metastatic disease, or when the cancer progresses despite the presence of RAI uptake. Multikinase inhibitors such as sorafenib and lenvatinib demonstrated progression free survival (PFS) benefit in patients with RAI refractory DTC and were approved by the United States Food and Drug Administration (US FDA). More recently cabozantinib was approved for patients who progressed on either of these two agents based on PFS benefit. However, it is important to remember that the diagnosis of RAI refractory disease does not always mean that the treatment needs to be offered. Generally, systemic treatment is offered when a doubling time is shorter than 1-4 years or when there is a significant symptom burden, but it can be tailored to individual patient’s overall tumor burden, symptoms, location of the disease, clinical contraindications and preference.19)
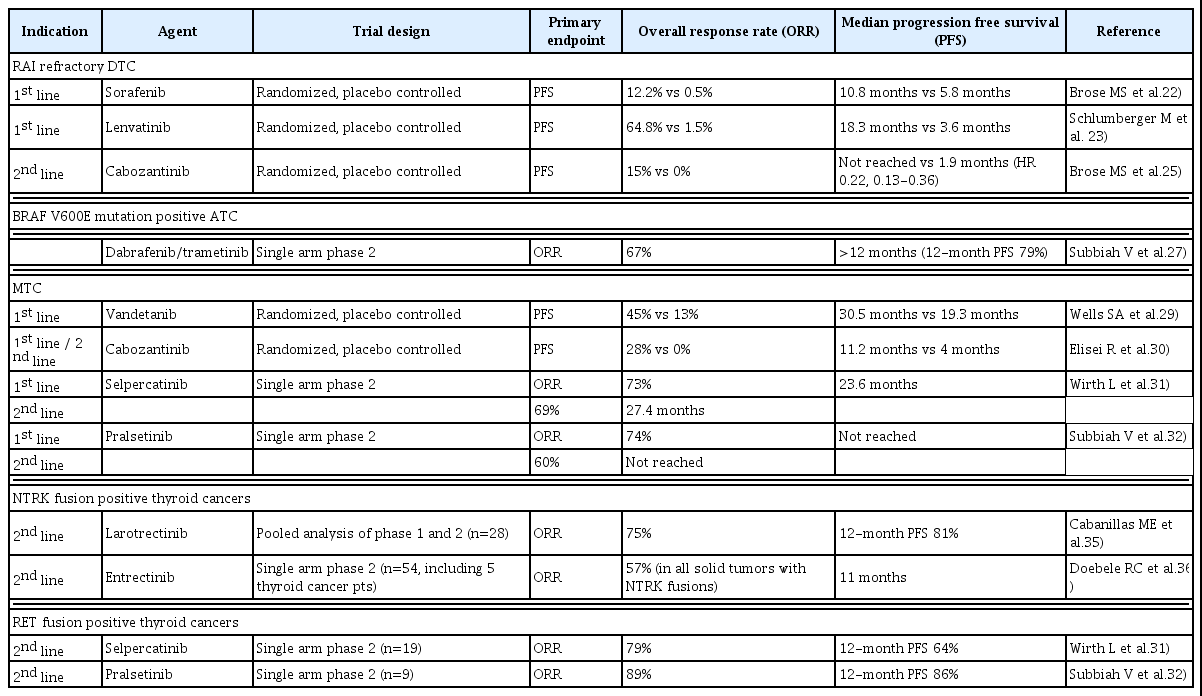
DTC has not been described as chemotherapy sensitive disease in traditional sense. In 2000s, series of phase 1 trials evaluating tyrosine kinase inhibitors such as cabozantinib, tipifarnib, sorafenib were initiated and showed preliminary activity in DTC patients.20) As expression of vascular endothelial growth factor (VEGF) and its receptors (VEGFR) was known to be elevated in thyroid cancers,21) and multikinase inhibitors targeting VEGFR pathway including sorafenib and lenvatinib entered clinical trials to evaluate their efficacy in DTC. Sorafenib was the first drug to be approved in RAI refractory DTC. In a phase 3 randomized, double- blind, placebo-controlled trial, sorafenib demonstrated statistically significant PFS benefit over placebo (HR 0.59, 95% CI 0.45-0.76, median PFS 10.8 vs. 5.8 months), with 41% reduction in the risk of progression or death.22) Lenvatinib was also evaluated in a phase 3 randomized, double-blind, placebo-controlled trial, and demonstrated significantly better PFS of 18.3 months over 3.6 months in placebo group (HR 0.21, 95%CI 0.14-0.31).23) Reported ORR was 65% for lenvatinib and 12% for sorafenib. Both trials included RAI refractory DTC patients defined by 1) at least one target lesion without iodine uptake, or 2) patients whose tumors had iodine uptake and progressed after one RAI treatment within 12 (Lenvatinib study) or 16 (sorafenib study) months, or 3) received cumulative RAI more than 600 mCi. Both agents demonstrated significant toxicity, although the pattern was slightly different. While there were common AEs such as fatigue and hypertension, hand-foot skin reaction, diarrhea, and rash were more prominent for sorafenib, whereas decreased appetite, weight loss, and proteinuria were reported more frequently for lenvatinib.
Cabozantinib is another multikinase inhibitor with activity against MET, which is implicated in resistance to VEGFR inhibitors such as sorafenib and lenvainib. In a multicenter phase 2 study, cabozantinib showed ORR of 40% and median PFS of 12.7 months in RAI refractory DTC patients who received at least one prior VEGFR targeting therapy.24) It was recently evaluated in a randomized, double-blind, placebo-controlled phase 3 trial in DTC patients who progressed during or after treatment up to two VEGFR tyrosine kinase inhibitors, and demonstrated significant PFS benefit over placebo (HR 0.22, 95%CI 0.13-0.36, median not reached vs. 1.9 months) and ORR of 15%.25) This study led FDA approval of cabozantinib for 2nd line treatment of RAI refractory DTC.
Poorly differentiated thyroid cancers/Anaplastic thyroid cancers
PDTC and ATCs have been treated with aggressive chemotherapy and radiation regimen. Intensive chemotherapy with doxorubicin and docetaxel combined with radiation has been reported to improve overall survival in a small retrospective case series, but the regimen is poorly tolerated.26) BRAF V600E mutation has been reported in up to 50% of ATC which can serve as a therapeutic target. A multi-center, open-label, nonrandomized, phase 2 trial to evaluate a combination of BRAF inhibitor and MEK inhibitor, dabrafenib and trametinib, demonstrated ORR of 67% in patients with confirmed BRAF V600E mutation with 12-month PFS of 79%.27) This result is very impressive, but a real-world experience with the same regimen does not seem to be as favorable as the reported outcome with ORR of 38% and median PFS of 5.2 months,28) which may reflect challenges of treating potentially sick and rapidly decompensating patients with ATC.
Medullary thyroid cancers
MTC do not respond to radioactive iodine treatment and activated RET kinase has been the main therapeutic target. Among different multikinase inhibitors explored in MTC, agents with activities in VEGFR and RET have demonstrated promising activities with ORR ranging between 30 to 50%.14) Vandetanib targets RET, VEGFR and EGFR signaling and was evaluated in a phase 3 randomized, double-blind, placebo-controlled clinical trial. The enrollment was not limited to patients with documented RET mutation, but the mutational status was confirmed by central testing. Vandetanib demonstrated significant PFS benefit over placement with HR of 0.46 (95%CI 0.31-0.69) with median PFS of 30.5 months over 19.3 months in the placebo group.29) In subgroup analyses of sporadic MTC patients, patients with RET M918T mutation had higher response rate to vandetanib compared to M918T mutation-negative patients (ORR 54.5% vs. 30.9%). Cabozantinib is another multikinase inhibitor that targets MET, VEGFR2 and RET. It was studied in a phase 3 randomized, double-blind, placebo-controlled trial for both treatment naïve and prior TKI treated MTC patients. The study demonstrated significant PFS benefit with HR 0.28 (95% CI 0.19-0.40) with median PFS of 11.2 months versus 4.0 months in placebo group. ORR was 40% in cabozantinib arm and 0% in placebo arm, and both RET mutation- positive and -negative group showed similar ORR (32% and 25% respectively). Approximately 20% of patients had prior TKI treatment in this trial.30) Both agents are deemed to have manageable toxicity profiles, although discontinuation rates were high (12% for vandetanib and 16% for cabozantinib) and grade 3-5 adverse events were common.
More recently, highly selective RET inhibitors such as selpercatinib and pralsetinib were developed to minimize off- target toxic effects of multikinase inhibitors. Selpercatinib is an ATP-competitive small molecule inhibitor of RET kinase and was designed to cover acquired gatekeeper resistance mutation at RET V804. Selpercatinib was investigated in an open label phase 1-2 trial and demonstrated ORR of 69% in 55 MTC patients previously treated with vandetanib, cabozantinib or both, including 9% of patients who achieved complete response. At one year, 86% of the responses were still on-going. Among patients who were treatment naïve, 73% of patients achieved objective response with 11% who had complete response. Main grade 3 or 4 adverse events observed were hypertension and increased liver enzymes with few treatment-discontinuation. QT prolongation on EKG was seen in 19% of patients, but no cardiac related serious adverse event was reported.31) Pralsetinib is another selective RET inhibitor designed to target activated RET kinase including the gatekeeper mutant V804. It was studied in an open label phase 1-2 trial and demonstrated ORR of 60% in 55 MTC patients previously treated with cabozantinib, vandetanib or both. ORR in 21 treatment-naïve MTC patients was 71%. Median PFS was not reached with estimated 1-year PFS rate of 81% after median follow-up of 15.1 months. Common grade 3-4 adverse events include hypertension, neutropenia and anemia and the latter two led to treatment interruptions in 15% of patients.32) These trials enrolled only RET mutation-positive patients, and both selpercatinib and pralsetinib represent great treatment options for RET mutation-positive MTC patients with excellent safety profiles.
Selective inhibitors for gene rearrangements in NTRK1/2/3 and RET
NTRK fusions encode TRK fusion proteins and can act as an oncogenic driver for various human cancers including thyroid cancers. NTRK1, NTRK2 and NTRK3 encodes for TRKA, TRKB and TRKC, respectively, and the TRK signal is known to play an important role in activation of neuronal survival and differentiation pathways. Gene rearrangements of NTRK1/2/3 can lead to fusion product of TRKs and well- known example includes ETV6-NTRK3 gene fusion which is seen in congenital fibrosarcoma and secretory carcinomas.33) Gene rearrangements in NTRK1 and NTRK3 are observed in 1% and 1.3% of PTCs, respectively.4) Larotrectinib is a potent and selective inhibitor of all three TRK proteins, TRKA, TRKB and TRKC and was investigated in an open- label phase 1-2 study for NTRK fusion-positive solid tumors. In 55 patients with NTRK fusion-positive cancers including five thyroid cancer patients, larotrectinib demonstrated ORR of 80% with 71% of responses ongoing at one year. The agent was very well tolerated with few grade 3 or 4 adverse events.34) A pooled analysis focusing on 28 thyroid cancer patients confirmed the activity with 75% ORR with one-year PFS rate of 81%. Of note, ORR of 29% was noted in 7 patients with ATC.35) Entrectinib is a potent inhibitor of ALK and ROS1 in addition to all TRK proteins. It was evaluated in an open-label phase 1-2 study for NTRK fusion-positive solid tumors and demonstrated ORR of 57% in 54 evaluable patients including five thyroid cancer patients. Median PFS was 11 months and overall grade 3-4 treatment-related adverse events were not common.36) Both drugs are approved by US FDA for treatment of NTRK fusion-positive solid tumors including thyroid cancers.
Selpercatinib and pralsetinib, highly selective RET inhibitors, were also evaluated in RET fusion-positive thyroid cancers, which accounts for 6.3 % of PTCs. Selpercatinib was evaluated in 19 patients with RET fusion-positive, previously treated thyroid cancer, and ORR was 79%. Activity was seen across multiple histologic types including PTC, PDTC, Hurthle cell carcinoma and ATC. At one year, 64% of patients were progression-free.31) Pralsetinib was evaluated in 9 patients with RET fusion-positive RAI refractory DTC, and ORR was reported to be 89% with 1-year PFS rate of 86%.32) Both drugs are approved by US FDA for treatment of RET fusion-positive thyroid cancers (Table 1).
Emerging therapy for thyroid cancers
Differentiated thyroid cancers
As previously mentioned, BRAF mutation is seen in 60% of PTC patients and it is rational to hypothesize BRAF inhibitors or BRAF inhibitor and MEK inhibitor combination would be effective for these patients. A multi-center, randomized phase 2 study of dabrafenib versus dabrafenib and trametinib combination has been performed for BRAF mutated RAI refractory PTC patients. The trial showed ORR of 50% for dabrafenib (n=26) and 54% for dabrafenib/trametinib (n=27) with median PFS of 11.4 months and 15.1 months, respectively. About 25% of patients had 1-3 prior lines of multikinase inhibitor therapy.37) The reported ORR is lower than that of lenvatinib (65%) but considering much lower ORR of lenvatinib reported in real-world experience reports (36%)38) and favorable safety profile, BRAF targeted agents can be an alternative treatment option for BRAF mutated DTC patients.
RAI remains to be the primary initial treatment strategy for metastatic DTC patients. Based on roles of activated MAPK pathway in de-differentiation and RAI refractoriness, strategies to restore RAI avidity by targeting the signaling pathway have been attempted. Most studies used MEK inhibitors or BRAF inhibitors and demonstrated an increase in RAI uptake in roughly 60% of patients. Objective tumor responses were observed following RAI treatment in mainly RAS or BRAF mutated patients, but responses in wild-type patients were also observed.39-41) Restoration of RAI avidity with use of TRK inhibitor42) has also been reported and sparked renewed interests in re-sensitization approaches.43)
Poorly differentiated thyroid cancers/Anaplastic thyroid cancers
Unlike many other solid tumors, immune checkpoint inhibitor has not demonstrated much activity in thyroid cancer in general. However, ATCs tend to have higher tumor mutational burden and high PD-L1 expression, which makes it an attractive target for immune checkpoint inhibitor therapy. Spartalizumab, an anti-PD1 antibody was evaluated in a single arm phase 2 study and demonstrated ORR of 19% in 42 patients. Interestingly, objective responses were only seen in PD-L1 positive patients and ORR for PD-L1 positive ATC patients was 29%. Responses were seen in both BRAF- mutant and wide type patients.44)
Immune checkpoint inhibitors can also be used as a salvage regimen after progression on targeted therapy agents. For patients who progressed on kinase inhibitor therapy, addition of pembrolizumab, another anti-PD1 antibody, showed ORR of 42% with median PFS of 3 months.45) Upfront combination of BRAF/MEK inhibition and immune checkpoint inhibitor was also explored for BRAF mutant ATCs. A single arm phase 2 trial of atezolizumab, vemurafenib and cobimetinib exhibited ORR of 71% among 17 patients treated.46) Immune checkpoint inhibitors are viable treatment options for ATC patients, although optimal sequence with targeted therapy needs to be investigated further.
Medullary thyroid cancers
Highly selective RET inhibitors such as selpercatinib and pralsetinib have activities against RET gatekeeper mutation at V804 but acquired resistance can still emerge through various mechanisms. A solvent front mutation at RET G810 has been proposed as a dominant resistance mechanism and was identified in patients who progressed on selpercatinib in clinical trials.47) Unlike gatekeeper mutations that modulate the accessibility of the kinase ATP-binding pocket, solvent front mutations cause a steric hindrance to the kinase inhibitors.48) Several investigational agents including TPX- 0046 (NCT04161391) and TAS0953/HM06 (NCT04683250) are being developed and evaluated in phase 1-2 trials to target solvent front mutations of RET.
Conclusion
Systemic treatment options for thyroid cancers have kept expanding over the last few years driven by developments in cancer genomics and immunology. For RAI refractory DTCs, cabozantinib was recently approved for patients who progressed on at least 1 line of prior VEGFR targeted therapy such as lenvatinib or sorafenib. Larotrectinib or entrectinib is available for NTRK1 or NTRK3 fusion positive thyroid cancers and selpercatinib or pralsetinib is for RET fusion positive thyroid cancers. For PDTC and ATC, dabrafenib and trametinib combination is approved for BRAF mutation positive cancers and demonstrated impressive activity. For MTCs, highly selective RET inhibitors, selpercatinib and pralsetinib, were added to conventional treatment options including vandetanib and cabozantinib. In the near future, we anticipate seeing the development of more precision oncology-based targeted therapy for specific genomic alterations and incorporation of immune checkpoint inhibitors in selected thyroid cancer patients.