Introduction
Fibrous dysplasia is a benign developmental bone condition in which abnormal fibrous tissues gradually proliferate and replace spongy bone, filling the medullary cavity. 1,2) Fibrous dysplasia of the orbit and skull base can invade the periorbital bone and induce orbital displacements and eye protrusion, consequently causing craniofacial deformities. 3) Therefore, appropriate resection followed by craniofacial reconstruction is necessary to treat fibrous dysplasia of the orbit and skull base. This study reports a case of facial fibrous dysplasia that developed in the frontal and ethmoid bones and superior orbital wall in a non-native patient that was successfully treated by radical resection followed by reconstruction using an autogenous split calvarial bone graft.
Case
A 21-year-old Uzbek male visited the present institution with a feeling that his left eye had started bulging 2 months ago. A clinical examination revealed downward and lateral displacements of the left eye by 5 mm and 2 mm, respectively, and eye protrusion by 3 mm (Fig. 1). No visual disturbance, malocclusion, or neurological symptoms were observed in the patient. Computed tomography (CT) images showed evidence of cortical thickening and osteosclerosis of the frontal bone and left ethmoid sinus (Fig. 2A, 2B). The patient was diagnosed with fibrous dysplasia based on these findings, and radical resection was planned after considering the patient’s age and location of the lesion.
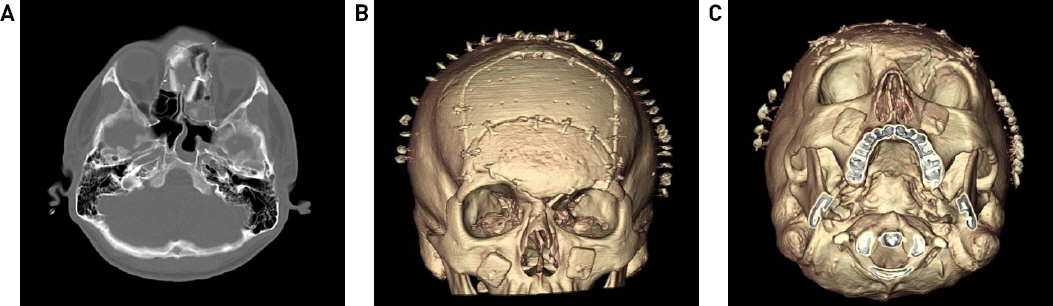
Fig. 2
Preoperative computed tomography. Focal bony sclerosis and thickening of the frontal bone and left ethmoidal sinus (A) axial view. (B) coronal view.
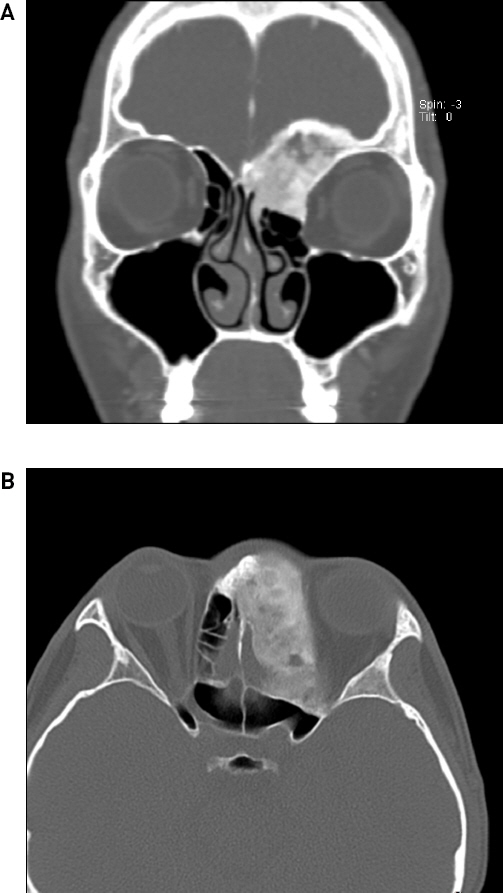
A bicoronal incision was made following induction with general anesthesia. Dissection was performed up to the glabellar area to secure a sufficient operative field. The lesion measured approximately 6.5 cm × 4 cm × 3.5 cm and involved the frontal and ethmoid bones and the superior orbital wall. An oscillating saw and rongeur were used to carefully perform radical resection of the lesion. Further, an air craniotome was used to harvest the frontal bone, in collaboration with the department of neurosurgery (Fig. 3). The harvested frontal bone was divided into inner and outer cortices using an oscillating saw, and the outer cortex was reserved for donor site coverage. A part of the inner cortex flap was excised into a convex triangle shape of approximately 1.5 cm × 2 cm and approximately 2 cm × 3.5 cm and fixed with a wire to the right ethmoid defect, left ethmoid bone and the bone defect area on the superior orbital wall. A new contour was formed by moving and fixing the inner cortex flap to the inner upper side so that the position of the newly formed upper orbital wall on the left side was similar to that of the right upper orbital wall. The remaining inner cortex flaps were cut in the shape of the frontal bone defect by maintaining the convex shape and then fixed with a wire to the newly formed superior orbital margin and the lower margin of the outer cortex flap used for donor site coverage (Fig. 4). A drain was inserted into the bicoronal incision area and wound closure was performed accordingly. On the axial view of the CT taken 8 days after the operation, the inner cortex flap fixed on the defect of ethmoid bones on both sides was well maintained while the 3D image showed that the frontal area and both superior orbital rims were found to maintain their symmetric contours (Fig. 5A, 5B, 5C). No specific complications such as vision problems, facial nerve disorders, and infections were observed in the patient. He has now been postoperatively followed up for 1 year and 5 months and has not experienced any recurrence. A clinical examination revealed a reduction in the downward displacement of the left eye from 5 mm to 1 mm and a reduction in lateral displacement from 2 mm to 0.5 mm. Exophthalmos also improved from 3 mm to 0.5 mm. The patient was satisfied with the functional and aesthetic outcomes of the surgery (Fig. 6). Written consent was received from the patient to publish this case report.
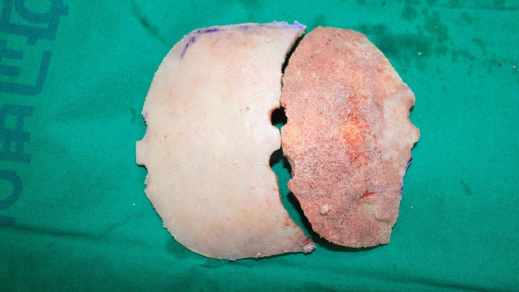
Fig. 3
Intraoperative photograph. Frontal bone was harvested following the radical resection of the fibrous dysplasia lesion in the fronto-orbital region.

Fig. 4
Intraoperative photograph. The harvested frontal bone was split and reassembled for reconstruction at the defect site.
Discussion
Fibrous dysplasia is a benign bone condition characterized by the replacement of normal bone by the connective tissues of fibrous bone. An activated mutation on the α-subunit of the G-signaling protein within osteoblastic cells is known to induce fibrous dysplasia by disrupting the functions of cells in the osteogenic lineage. 1,2) Fibrous dysplasia usually develops in childhood and accounts for 2.5% of all bone tumors and 7.5% of benign bone tumors. 3-5) It is clinically classified as monostotic or polyostotic. Seventy percent of patients with fibrous dysplasia have monostotic lesions, and craniofacial involvement is observed in 10% of monostotic lesions and 50-100% of polyostotic lesions. 3)
Swelling and facial asymmetry are the most common symptoms of craniofacial fibrous dysplasia. 6,7) Different signs and symptoms are observed depending on the anatomical location involved. 3) Involvement of the temporal bone or otic capsule can lead to hearing loss, and that of the frontal, sphenoid, ethmoid, and maxillary bone can lead to sinusitis and nasal congestion. 6,8) Cranial bone or orbital involvement can lead to headaches, orbital dystopia, vision loss, paresthesia, eye protrusion, epiphora, and blindness. 8,9)
No clear guidelines have been established for the treatment of craniofacial fibrous dysplasia. 3) Surgery is the only option for cranial fibrous dysplasia, excluding for those lesions that develop at the central cranial base with involvement of major vessels and cranial nerves. 3,7) In cases where surgery is not possible, a radiologic examination is performed and symptoms are monitored accordingly. There have been attempts to pharmacologically treat craniofacial fibrous dysplasia using potent osteoclast inhibitors such as pamironate and bisphosphonate; however, their therapeutic effects are yet to be verified. 3)
Whether surgical treatment is more appropriate than conservative or radical treatment remains controversial. 7) When choosing a treatment method, it is necessary to aim for not only achievement of functional and aesthetic improvements but also to minimize the risk of recurrence and reoperation. The patient’s age, lesion location, scope of lesion, orbital displacement, patient preferences, and the level of experience of the surgical team must also be considered before the initiation of treatment. 7,10)
Radical resection has been reported to achieve lower recurrence and reoperation rates in craniofacial fibrous dysplasia than conservative treatment. 11) Complete resection of a craniofacial fibrous dysplasia lesion is necessary since malignant changes of fibrous dysplasia have been reported, albeit rarely. 12) In cases of lesions in the fronto-orbital region accompanied by orbital dystopia such as the one in this case report, radical resection is absolutely needed since the lesions can progress toward the inside of the eye or the cranial base to apply pressure on the optic canals or the neurovascular structures of the superior orbital fissure, consequently causing vision loss and serious complications. 3) A recent study has also reported radical resection to be the most appropriate method of treatment for adult patients with zone I, II, and IV lesions under the Chen and Noordhoff grading system. 7)
However, it has been reported that conservative procedures such as reduction burring resolved functional and aesthetic problems and minimized facial changes that occurred over the course of development in patients aged less than 7 years without vision problems more effectively than radical resection. 7) It has also been reported that early surgery before skeletal maturity reduces the rate of recurrence afterwards. 13) However, if a lesion has already invaded the fronto-orbital region and acute visual deficits have occurred within one month as was the case with the patient in this report, radical resection is still necessary, regardless of age. 7)
It is important to appropriately determine the globe position and maintain the orbital volume when reconstructing the calvarial bone in the fronto-orbital region. 3) Aesthetic abnormalities such as dystopia can be corrected once an orbital rim has been appropriately formed, and a sufficient orbital volume must be secured to prevent functional globe problems such as diplopia and exophthalmos. 14-15)
In this case report, the surgical site was widely exposed through a bicoronal incision, and a sufficient size of autogenous frontal bone was harvested for reconstruction. The harvested frontal bone was reassembled to match the shape of the defect site using a split calvarial bone graft and was transplanted onto the sites of defect on the frontal bone and superior orbital wall and rim to achieve convexity similar to that on the side opposite to the lesion. Using this approach, an appropriate orbital contour and volume could be obtained. In cases of lesions in the frontal sinuses or ethmoid sinuses where there is a potential risk of contamination or in lesions accompanied by nearby defects in the calvarial bone, using an autogenous bone graft as was done in this case may more effectively lower the risk of infections as opposed to using alloplastic materials.
Many factors must be considered during craniofacial bone reconstruction. Several surgical methods have been proposed to predict the appropriate graft shape and reduce the operation time. In a recent study, Ahn et al. introduced a reconstruction approach in which a rapid prototyped model created by a three-dimensional printer was used to plan the shape of an autologous calvarial bone graft following the radical resection of fibrous dysplasia in the zygomaticomaxillary region. 10)
With exceptions, radical resection and reconstruction is necessary for craniofacial fibrous dysplasia and especially so in lesions in the fronto-orbital region to prevent aesthetic and functional complications, recurrences, and malignant changes. This paper reports a case of fibrous dysplasia that occurred in the fronto-orbital region, which was successfully treated by radical resection followed by reconstruction using an autogenous bone graft. The procedure achieved satisfactory functional and aesthetic outcomes.