Introduction
Paraganglioma is a rare benign tumor that develops from the skull base to the pelvis in the paraganglion system.
1-
7) Paraganglioma is most common in the abdomen, followed by the chest and head and neck.
2,
3,
6) Paraganglioma accounts for 0.6% of the all the benign tumors affecting the head and neck region.
3) Head and neck paraganglioma is usually slow growing and non-secretory.
6) In the head and neck region, it occurs mainly in the temporal bone, jugular foramen, vagus nerve, or carotid body.
3,
4,
6) Herein, we report a case of paraganglioma of the submandibular region that has not been reported.
Case report
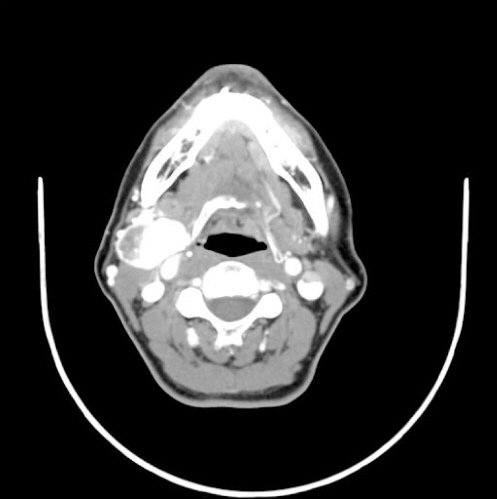
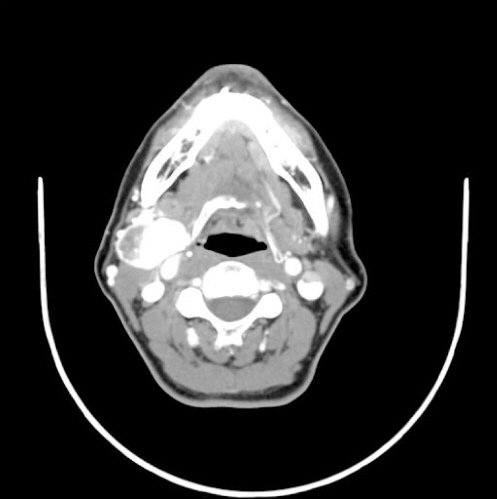
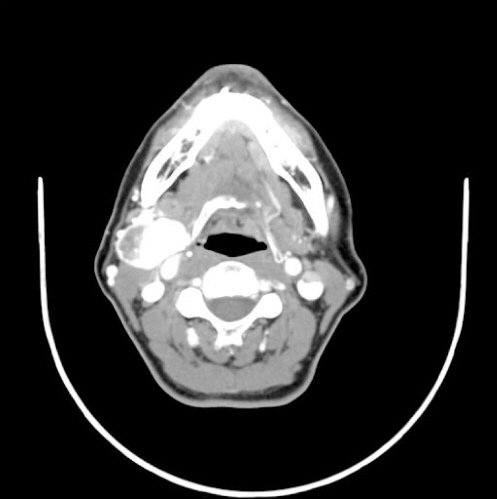
An age 61 female complained of a painless, slowly growing mass in right submandibular region for two years. She had no pain, fever, or other symptoms. Physical examination showed a firm, non-tender, 3 cm mass below the angle of the mandible. Other examinations, including cranial nerve examinations and fiberoptic laryngoscopy examinations, were normal. Neck ultrasonography (US) showed a 3.8 × 2.2 cm oval well circumscribed intermediate echoic mass of the right submandibular area. US-guided fine-needle aspiration cytology (FNAC) was diagnosed as salivary gland neoplasm of uncertain malignant potential. Neck computed tomography (CT) scan demonstrated a 3.5 × 3.5 × 2.5 cm strongly enhancing mass in the right submandibular area (
Fig. 1). Based on the above results, our preoperative diagnosis was cervical neck hemangioma.
Fig. 1
Neck computed tomography scan demonstrates a 3.5 x 3.5 x 2.5 cm strongly enhancing mass in the right submandibular area.
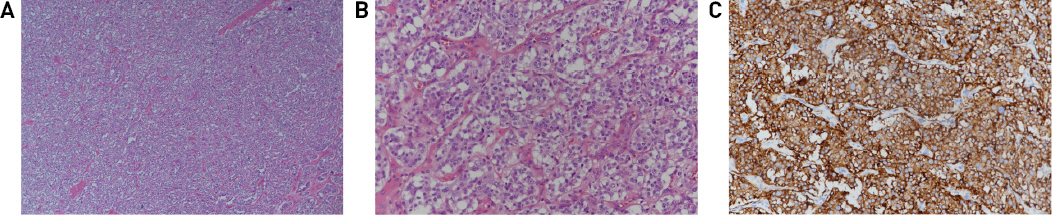
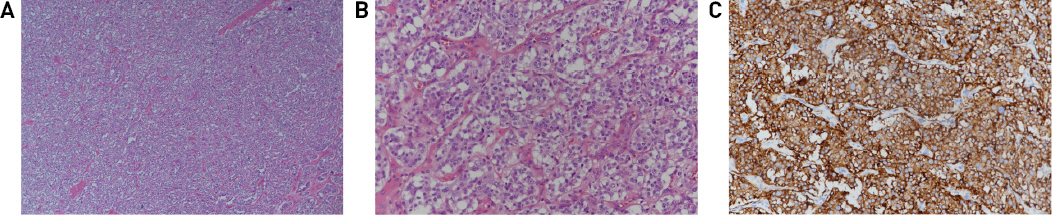
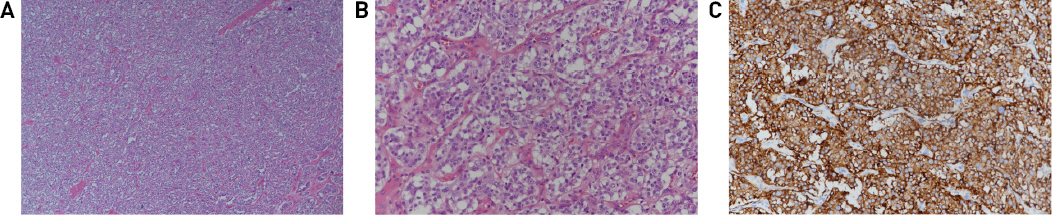
Right neck mass excision was performed under general anesthesia. The cervical neck mass was easily separated into submandibular gland, and no connection with surrounding structures such as carotid artery. The final histopathologic result was diagnosed with paraganglioma (
Fig. 2). The immunohistochemistry stains for synaptophysin and S-100 protein were positive (
Fig. 2). After the diagnosis of cervical neck paraganglioma, family history, abdomen CT, urinary catecholamine test, hormone test and succinate dehydrogenase gene mutation test were performed in the Department of Internal Medicine. All test results were normal. The patient is constantly being followed up without recurrence.
Fig. 2
(A) Growth patterns include organoid or trabecular. The tumor nests are separated by fibrovascular network (Zellballen pattern) (Hematoxylin and eosin stain, x40). (B) The tumor cells have abundant granular eosinophilic cytoplasm and slight atypical nuclei. Mitotic figures are very rare (Hematoxylin and eosin stain, x200). (C) The immunohistochemistry stains for synaptophysin is positive.
Discussion
Paraganglioma is rare neuroendocrine tumor arising from the paraganglia of the autonomic nervous system.
1-
7) Paraganglioma occurs in the carotid body (most common), jugular foramen, and vagus nerve in the head and neck region.
3,
4,
6) There have been no reports of paraganglioma in the submandibular region. Paraganglioma is classified into sporadic, familial, and related to high altitudes, of which sporadic form is the most common.
1) This patient was also diagnosed as sporadic form because there was no abnormality in the family history and succinate dehydrogenase gene mutation test.
The symptoms of paraganglioma vary depending on the location and size of occurrence.
1-
3) In the head and neck, they show symptoms such as mass, local discomfort, otalgia, tinnitus, facial weakness, dysphagia, hoarseness, sycope and a rare Horner’s syndrome.
1-
3) This patient complained only of the painless, non-tender mass below the angle of the mandible.
The diagnostic method for paraganglioma is radiologic examinations.
1-
7) CT and magnetic resonance imaging (MRI) facilitate evaluation of the site of origin, vascularity of the lesion, extent of the lesion, and its relationship to adjacent structures.
1,
3) In the CT scan, paraganglioma is markedly well contrasted.
1-
3,
5) MRI can demonstrate an inhomogeneous hyperintense image from vascular fast flow.
1,
2) In this case, additional abdominal CT was performed after surgery to identify multiple paraganglioma or metastasis. Differential diagnosis for paraganglioma of the submandibular region should include submandibular lymphadenopathy, tuberculous lymphadenitis, neck abscess, vascular malformation, submandibular gland tumor, and schwannoma.
1)
Treatment of paraganglioma in head and neck region include surgery, radiotherapy, and proton therapy.
1-
7) Surgery is the treatment of choice for the management of head and neck paraganglioma.
1,
3,
7) In addition, regional cervical lymph node should be included in the primary specimen to rule out the malignant transformation.
3) Small tumors can be easily removed without damage to the vascular structures or nerves, as with our patient.
1,
3,
7) However, for large tumors, the probability of neurovascular complications after surgery is markedly high.
1-
3,
7) Radiotherapy can be considered for unresectable tumors, high-risk patients, incompletely resected tumors, local recurrence, and metastatic lesions.
1,
2) Surgery and radiotherapy are the main treatments, but recently there have been reports of effective and safe tumor control in head neck paraganglioma with proton therapy.
7)
Paraganglioma is the most benign tumor, but it can be malignant from 5% to 20%.
1,
2) Malignant paraganglioma can also cause regional and distant metastasis.
1,
2)
Conclusion
Paraganglioma of the submandibular region is an extremely rare disease. This case highlights paraganglioma as a rare differential diagnosis for submandibular gland tumors.