신경 섬유종증 1형 환자의 양측 후두 신경통: 증례보고
Bilateral Occipital Neuralgia in a Patient with Neurofibromatosis Type 1: A Case Report
Article information
Abstract
= Abstract =
Plexiform neurofibromas (PNFs) represent an uncommon variant (30%) of neurofibromatosis type 1 (NF-1), in which neurofibromas arise from multiple nerves as bulging and deforming masses involving connective tissue and skin folds. We report the case of a 17-year-old man with known NF-1 presenting with bilateral occipital neuralgia that began in his late adolescence. His chief complaint was radiating pain in the occiput induced by protective helmet wear when riding alpine skiing. Craniofacial magnetic resonance imaging (MRI) confirmed the presence of fusiform masses arising from the bilateral greater occipital nerves. Histopathological examination of the biopsy samples showed PNFs. After surgical treatment, the patient’s symptoms completely improved. Unlike cutaneous neurofibromas, PNFs have different clinical characteristics and have the risk of malignant mutations. Correct diagnosis and adequate surgical treatment are necessary for PNFs.
Introduction
Neurofibromatosis type 1 (NF-1) is a autosomal dominant disorder caused by germline mutations in the NF-1 tumor suppressor gene, affecting approximately 1 in 2500 to 1 in 3000 people worldwide.1,2) NF-1 is characterized by multiple pigmentary lesions such as café-au-lait macules, axillary freckling and tumoral growth along nerves, called neurofibromas.3) There are four subtypes of neurofibromas: cutaneous, subcutaneous, plexiform, and spinal. Plexiform neurofibromas represent an uncommon variant of NF-1. They differ from cutaneous neurofibromas because they arise from multiple nerve fascicles and can grow along the length of a nerve; hence, the lesions are clinically described as “bags of worms.” These tumors can also extend into the surrounding structures, causing substantial pain and bone destruction. Importantly, plexiform neurofibromas (PNFs) have a lifetime risk of malignant transformation.4) Surgical removal is the best therapeutic option for treating symptomatic lesions. We report a case of PNF arising from the bilateral greater occipital nerves, which presented with classic hallmarks of NF-1.
Case report
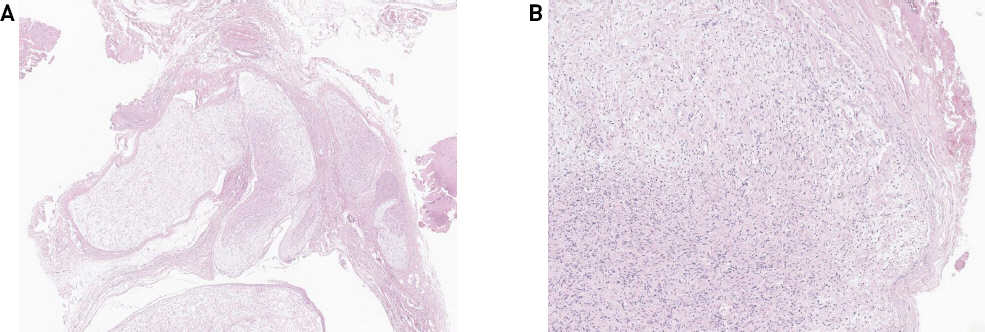
A 17-year-old boy visited our outpatient clinic presenting pain with palpable masses in his bilateral occipital region that started 6 months ago. He had been previously diagnosed with NF-1 for multiple cutaneous neurofibromas, café-au-lait macules over his entire body, long bone dysplasia, and Lisch nodules. In addition, genetic mutation of the NF1 gene on 17q11.2 was noted. However, there was no family history of neurofibromatosis. He presented with congenital below-knee amputation on his right lower leg and had undergone Boyd amputation on the left side for congenital foot deformity by orthopedic surgeon. For the palpable occipital masses, the orthopedic surgeon referred him to our department for evaluation and surgical treatment. On physical examination, he had a 3-cm round protruding lesions at the bilateral occiput areas, which was soft and non-fluctuant without pigmentation on the overlying skin. The patient had no neurological deficits. He complained of intermittent neuralgia in the occiput area due to these lesions while wearing a helmet when playing the alpine skiing. There was no prior medication history for intermittent pain. Ultrasonographic examination revealed multiple variable-sized oval to fusiform hypoechoic nodules arranged in a row, in the bilateral occiput area. Magnetic resonance imaging (MRI) showed approximately 3.0-3.5 cm sized T2 high signal masses along the bilateral occipital nerve, which is suggestive of a neurogenic tumor (Fig. 1).
Preoperative magnetic resonance imaging showing the mass. (A) The lobulated high-signal-intensity masses are shown in the axial view of T2-weighted image (red arrows), (B) in the sagittal view of a T2-weighted image (red arrow).
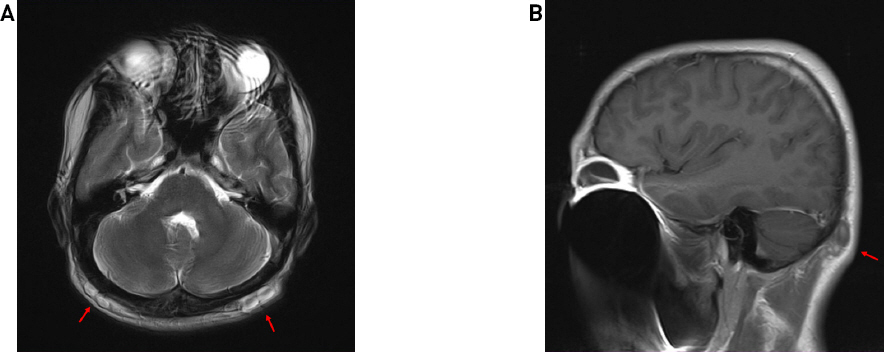
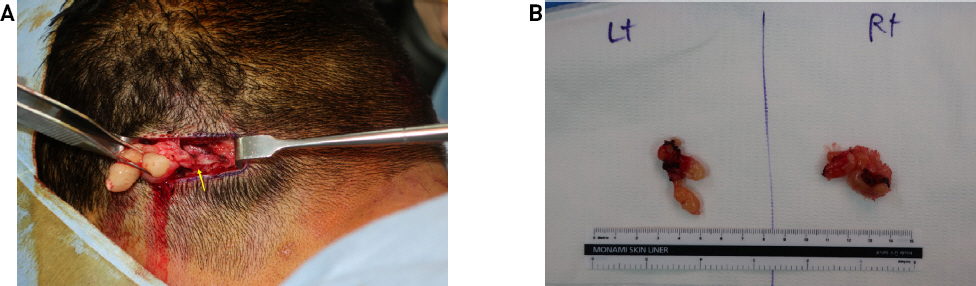
Surgical excision was performed under general anesthesia. Intraoperatively, transverse linear incisions were made directly on the bilateral masses. They were located deep under the subcutaneous layer. The greater occipital nerves were identified running next to the greater occipital arteries, and several 0.5-1 cm sized masses formed clusters along the branch of the great occipital nerve (Fig. 2A). Involvement of greater occipital nerves (GON) with the masses was identified, and small branch of GON was ligated with a hemoclip. Two masses were totally excised without sacrificing main branch of GON and sent for histology (Fig. 2B). Histopathological examination of the biopsy samples revealed PNF. The plexiform growth pattern showing multiple tumoral nodules, each composed of loose spindle cells with short, elongated, wavy nuclei embedded in a mucinous stroma (Fig. 3). Follow-up examination showed complete wound healing without sensory loss and the numerical rating scale (NRS) score was reduced from 6 to 0, 2 months postoperatively.
Intraoperative photograph. (A) Lobulated masses hanging along the branch of the greater occipital nerve (yellow arrow), (B) Surgical specimen.
Discussion
PNFs occur from birth in 25% to 50% of children with NF-1,5) and can continue to grow during adolescence and early adulthood.6) These lesions reveal early in life and tend to develop into malignant peripheral nerve sheath tumors (MPNSTs) in 2% to 16% of cases.4) It is an unencapsulated lesion that infiltrates the surrounding soft tissue, resulting in a fusiform appearance.6) PNFs are usually diagnosed clinically by evaluation of the typical features, and histopathology is helpful in ruling out malignant transformation.
In our case, PNFs were found relatively late for symptoms occipital neuralgia, and the MRI conducted at the age of 10 years showed no lesions, but the lesions grew around the age of 17 years. Previously, cases of PNF with involution to the surrounding soft tissue and apparent fusiform appearance have been reported.7,8) However, our patient did not show skin lesions, and the lesions were located deep beneath the muscle, resulting in an appearance different from the usual cutaneous neurofibroma or PNFs.
PNFs are located most commonly in the craniofacial region,9) and are usually found along the course of a major nerve trunk, the ophthalmic division in the face.10) In Helmholtz and Cushing’s first description, as detailed by Scott,11) the location of the PNF was on the forehead and temporal region. Although the forehead and the distribution along the trigeminal nerve are the most common locations, there have been a few reports of PNF occurring at the occiput.10) Various clinical symptoms can be observed depending on the prevalent locations. The main symptoms are ocular motility discomfort, dyspnea and respiratory failure from upper airway compression, neurological deficits from cranial nerve compression, social contraction, and other mood disorders resulting from facial disfigurement;12) in such cases, the patients are alpine skiers, complaining of sharp shooting pain caused by pressing the lesion when wearing a protective hat, and the symptoms recover after surgery. Any apparent deformation was barely noticeable because the masses were covered by hair.
Occipital neuralgia is a painful condition affecting the posterior scalp in areas where the greater occipital nerve (GON), lesser occipital nerve (LON), or third occipital nerve (TON) innervate. Most cases of occipital neuralgia are considered idiopathic, but they can be associated with other causes, such as previous skull base surgery, trauma, and nerve compression by other structures.13) Scalp masses can cause occipital neuralgia, but their incidence is low and preoperative diagnosis may be difficult, among benign tumors of peripheral nerves, the group originating from Schwann cells can be divided into two subtypes: schwannomas and neurofibromas. Cases have been reported for occipital neuralgia caused by neurogenic tumors, which improved after surgical resection of the mass.14,15)
In conclusion, occipital PNF is a rare benign tumor associated with NF-1. Without visual soft tissue deformation, deep-seated PNFs can be difficult to distinguish from other benign masses. Proper surgical excision and pathological diagnosis are required. Our case report may serve as a reference for PNF in the greater occipital nerve, as it was successfully treated without nerve damage. Long-term follow-up is recommended to determine whether there is a recurrence or malignant transformation.
Patient consent
The patient provided written informed consent for the publication and use of the images.
Acknowledgments
The study was approved by the Institutional Review Board of Seoul National University Hospital (IRB No. H- 2106-104-1227) and performed in accordance with the principles of the Declaration of Helsinki. Written informed consent was obtained.