몰입성 하마종의 피씨바닐 경화요법 치료 효과
Efficacy of Picibanil Sclerotherapy in Treatment of Plunging Ranula
Article information
Abstract
= Abstract =
A plunging ranula is a pseudocyst caused by mucus secreted from the sublingual glands, and it is mainly observed on the mouth floor. Nowadays, sclerotherapy using picibanil has been performed instead of invasive surgical treatment, and studies are reporting safe and effective outcomes. In our study, more than 92% of the 25 patients had marked response after picibanil sclerotherapy, and no serious complications were observed. Picibanil sclerotheraphy can be considered as the primary treatment of plunging ranula for patients who refuse surgery under general anaesthesia.
Introduction
A plunging ranula is a pseudocyst caused by mucus secreted from the sublingual glands, and it is mainly observed on the submandibular area extending through mylohyoid muscle.1) For the treatment of plunging ranula, surgical removal is widely used as an initial treatment. Recent studies recommended sublingual gland (SLG) excision with ranula evacuation than simple excision.2) There is also report that partial SLG excision reduces the operation time and is equivalent in terms of recurrence rates compared to the complete SLG excision.3)
Simple ranula can be removed with a transoral approach. However, cervical incision is unavoidable for plunging ranula due to the location of the tumor. Children, older adults, or patients who are worried about surgical scars prefer non- invasive treatment. Surgical removal of SLG is currently the main treatment for ranulas; however, incomplete resection, recurrence after surgery, and damage to surrounding structures, such as the hypoglossal nerve and Wharton’s duct, may lead to complications. Therefore, sclerotherapy has been performed in the recent years instead of invasive surgical treatment, and studies are reporting favorable outcomes.4) Picibanil (Chugai Pharmaceutical Co., Tokyo, Japan) is a drug that has been used for anti-cancer immuno- therapy. The administration of picibanil into lesions leads to strong inflammatory reactions in the tissues and induces secretion of various cytokines to promote adhesion.5) Based on these effects, Ogita et al. reported outstanding effects of picibanil for the treatment of lymphatic malformation.6) Ranulas are thin membrane-enclosed cystic masses that are structurally similar to lymphatic malformation, and studies have reported safe and effective results with picibanil as a treatment for ranulas.4) Thus, the purpose of our case series study was to assess the effects of picibanil sclerotherapy for plunging ranula.
Methods
Patients
The medical records of 25 patients, who were diagnosed with plunging ranula and received picibanil sclerotherapy as the primary treatment by a single surgeon (HAS) in the National Health Insurance Service Ilsan hospital from January 2010 to December 2019, were retrospectively analyzed. The diagnosis of plunging ranula was made through physical and radiological examinations. All patients who visited the hospital for neck swelling underwent CT scans to confirm the lesions. A hypoechoic cystic mass was observed around the sublingual and submandibular glands on CT, and the maximal diameter of the lesion on axial cut CT image of the area, where the cystic lesion was visible, was measured to assess the legion size. Once the cyst was observed, surgical and sclerotherapy treatment methods and progressions were explained to the patients. Next, an ultrasonography guided aspiration was performed on patients who wanted sclerotherapy in an outpatient clinic.
Procedures
Picibanil was administered into the lesion as follows. A dose of 0.1 mg of the picibanil (1KE) was dissolved in 10 mL of normal saline (1KE/10ml) and prepared in a syringe in advance. Ultrasonography was performed to confirm the location and size of the cystic lesion. Local anaesthesia was then induced on the lesion site using 1% lidocaine, and the liquid was aspirated as much as possible using a 22G angiocath peripheral venous catheters. After which, picibanil of the same volume as the aspiration volume was injected. No leakage or missed injection was observed when picibanil was administered. After 1 month of treatment, a decrease in the neck swelling was assessed as the primary outcome. Afterwards, the patients were instructed to re-visit the hospital once neck swelling recurred. If there were no complications, the patient was followed up 4-6 months after treatment to re-assess the treatment site.
The results for treatment were defined as follows. Cases of no mass observed during examination, manipulation, and imaging was defined as a complete response (CR). When the size of the mass decreased by 50% or more compared to that before treatment, it was defined as a marked response (MR). If the decrease in size was less than 50%, it was defined as a partial response (PR).
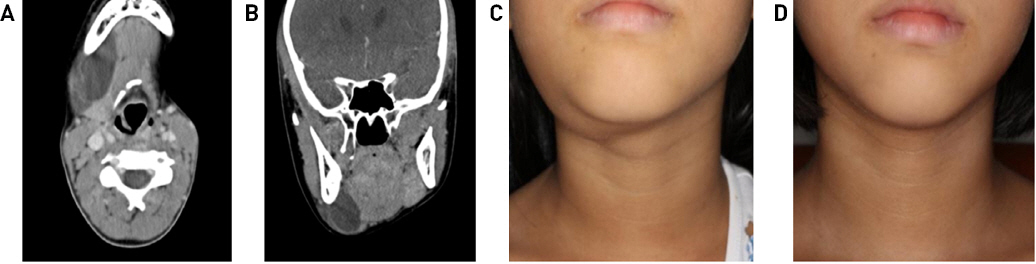
Results
The male to female ratio and mean age of the patients were 15:10 and 22.4 (7-24) years, respectively. The longest diameter of the plunging ranula was measured on computed tomography (CT) scan performed before sclerotherapy, and the average diameter was 4.39 (2.8-6.3) cm. The average aspiration volume was 11.36 (3-26) mL, and all lesions were localized above the hyoid bone (De serres type 2). Eleven patients were cured after single injection whereas six, five, and three patients received 2, 3, and 4 injections, respectively. The mean follow-up period of the patients was 18.8 (1-92) months. The treatment results of patients are summarized in Table 1. On the last day of visit, 13 (52%), 10 (40%), and 2 (8%) patients had CR, MR, and PR, respectively. In 23 (92%) patients, an effective outcome of MR or better was observed. There were no cases of rupture during administration, and 3 (12%) patients complained of lesion pain after sclerotherapy. No other serious complications were observed (Fig. 1).
Discussion
In our study, more than 92% of the patients had MR or better outcomes after picibanil sclerotherapy, suggesting that the treatment was very effective. Similarly, Kono et al. also reported a CR response rate close to 90%.4) In previous studies, a recurrence rate of 50% or greater was observed after a single injection, and in our study, we also injected picibanil twice or more in 56% (14/25) of patients. Although at least two injections were required for a satisfactory response, the treatment seemed adequate in that the procedure was simple and it led to a low rate of complications.
Ohta et al. reported that neutrophils and monocytes increased after picibanil injection, inducing the secretion of cytokines, including interleukin-6, interleukin-8, interferon-γ, and tumour necrosis factor-α.7) This caused a strong inflammatory reaction to the cyst wall, leading to drainage and cyst adhesion. A plunging ranula is uniloculated, and the cyst wall is composed of fibrous tissue. Thus, the drug spreads easily into the cyst and causes an effective response.8) Although picibanil has limited side effects, it is a mixture of weakly toxic group A Streptococcus pyogenes and penicillin G potassium. Therefore, skin reaction tests need to be performed in patients with suspected penicillin allergy to reduce the likelihood of anaphylactic reactions. The complications of picibanil injection is minimal, with no major side effects in previous studies and there was also no difference of injection dose between adults and child.9,10)
Conclusion
Currently, surgery is the primary treatment for plunging ranulas. However, sclerotherapy using picibanil is effective as it can be easily performed in an outpatient clinic, has excellent treatment outcomes, and has no major adverse side effects. This study was a small-scale case series of 25 patients, and there were limitations in verifying the effects of the drug with the retrospective study design. Clinical studies employing other designs, such as prospective research with increased number of patients, would be necessary in the future.