1)) Davies L, Welch HG. Increasing incidence of thyroid cancer in the United States, 1973-2002. JAMA. 2006;295:2164-2167.


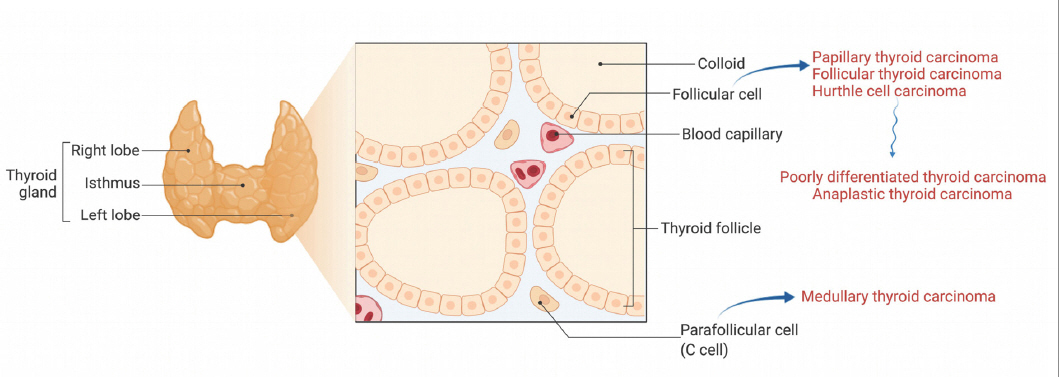
3)) Shah JP. Thyroid carcinoma:epidemiology, histology, and diagnosis. Clin Adv Hematol Oncol. 2015;13:3-6.

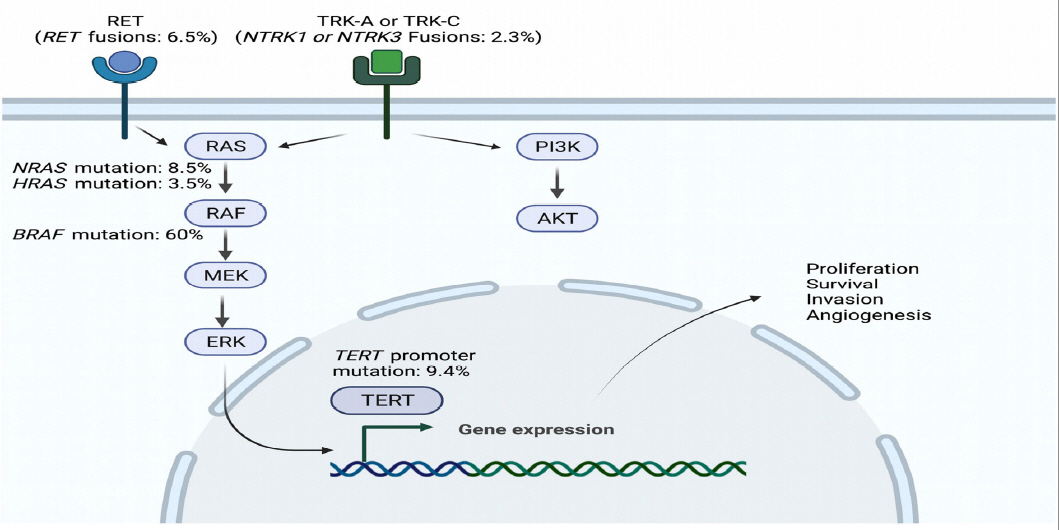
4)) Cancer Genome Atlas Research N. Integrated genomic characterization of papillary thyroid carcinoma. Cell. 2014;159:676-690.


8)) Xing M. BRAF V600E mutation and papillary thyroid cancer. JAMA. 2013;310:535.


9)) Xing M, Alzahrani AS, Carson KA, Shong YK, Kim TY, Viola D, et al. Association between BRAF V600E mutation and recurrence of papillary thyroid cancer. J Clin Oncol. 2015;33:42-50.


11)) Yip DT, Hassan M, Pazaitou-Panayiotou K, Ruan DT, Gawande AA, Gaz RD, et al. Preoperative basal calcitonin and tumor stage correlate with postoperative calcitonin normalization in patients undergoing initial surgical management of medullary thyroid carcinoma. Surgery. 2011;150:1168-1177.


12)) Passos I, Stefanidou E, Meditskou-Eythymiadou S, Mironidou-Tzouveleki M, Manaki V, Magra V, et al. A Review of the significance in measuring preoperative and postoperative carcinoembryonic antigen (CEA) values in patients with medullary thyroid carcinoma (MTC). Medicina (Kaunas). 2021;57.

14)) Hadoux J, Pacini F, Tuttle RM, Schlumberger M. Management of advanced medullary thyroid cancer. Lancet Diabetes Endocrinol. 2016;4:64-71.


17)) Grubbs EG, Ng PK, Bui J, Busaidy NL, Chen K, Lee JE, et al. RET fusion as a novel driver of medullary thyroid carcinoma. J Clin Endocrinol Metab. 2015;100:788-793.


21)) Klein M, Vignaud JM, Hennequin V, Toussaint B, Bresler L, Plenat F, et al. Increased expression of the vascular endothelial growth factor is a pejorative prognosis marker in papillary thyroid carcinoma. J Clin Endocrinol Metab. 2001;86:656-658.


23)) Schlumberger M, Tahara M, Wirth LJ, Robinson B, Brose MS, Elisei R, et al. Lenvatinib versus placebo in radioiodine-refractory thyroid cancer. N Engl J Med. 2015;372:621-630.


25)) Brose MS, Robinson B, Sherman SI, Krajewska J, Lin CC, Vaisman F, et al. Cabozantinib for radioiodine-refractory differentiated thyroid cancer (COSMIC-311):A randomised, double-blind, placebo-controlled, phase 3 trial. Lancet Oncol. 2021;22:1126-1138.


26)) Foote RL, Molina JR, Kasperbauer JL, Lloyd RV, McIver B, Morris JC, et al. Enhanced survival in locoregionally confined anaplastic thyroid carcinoma:a single-institution experience using aggressive multimodal therapy. Thyroid. 2011;21:25-30.


27)) Subbiah V, Kreitman RJ, Wainberg ZA, Cho JY, Schellens JHM, Soria JC, et al. Dabrafenib and trametinib treatment in patients with locally advanced or metastatic BRAF V600-mutant anaplastic thyroid cancer. J Clin Oncol. 2018;36:7-13.


29)) Wells SA Jr, Robinson BG, Gagel RF, Dralle H, Fagin JA, Santoro M, et al. Vandetanib in patients with locally advanced or metastatic medullary thyroid cancer:A randomized, double-blind phase III trial. J Clin Oncol. 2012;30:134-141.


32)) Subbiah V, Hu MI, Wirth LJ, Schuler M, Mansfield AS, Curigliano G, et al. Pralsetinib for patients with advanced or metastatic RET-altered thyroid cancer (ARROW):a multi-cohort, open-label, registrational, phase 1/2 study. Lancet Diabetes Endocrinol. 2021;9:491-501.


35)) Cabanillas ME, Drilon A, Farago AF, Brose MS, McDermott R, Sohal D, et al. 1916P Larotrectinib treatment of advanced TRK fusion thyroid cancer. Annals of Oncology. 2020;31:S1086.

36)) Doebele RC, Drilon A, Paz-Ares L, Siena S, Shaw AT, Farago AF, et al. Entrectinib in patients with advanced or metastatic NTRK fusion-positive solid tumours:integrated analysis of three phase 1-2 trials. Lancet Oncol. 2020;21:271-282.


37)) Shah MH, Wei L, Wirth LJ, Daniels GA, Souza JAD, Timmers CD, et al. Results of randomized phase II trial of dabrafenib versus dabrafenib plus trametinib in BRAF-mutated papillary thyroid carcinoma. Journal of Clinical Oncology. 2017;35:6022-6022.

38)) Locati LD, Piovesan A, Durante C, Bregni M, Castagna MG, Zovato S, et al. Real-world efficacy and safety of lenvatinib:Data from a compassionate use in the treatment of radioactive iodine-refractory differentiated thyroid cancer patients in Italy. Eur J Cancer. 2019;118:35-40.


39)) Ho A, Grewal R, Leboeuf R, Sherman E, Pfister D, Deandreis D, et al. Selumetinib-enhanced radioiodine uptake in advanced thyroid cancer. New England Journal of Medicine. 2013;368:623-632.


40)) Rothenberg S, Daniels G, Wirth L. Redifferentiation of iodine-refractory BRAF V600E-mutant metastatic papillary thyroid cancer with Dabrafenib-response. Clinical Cancer Research. 2015;21:5640-5641.


42)) Groussin L, Clerc J, Huillard O. Larotrectinib-enhanced radioactive iodine uptake in advanced thyroid cancer. N Engl J Med. 2020;383:1686-1687.


43)) Buffet C, Wassermann J, Hecht F, Leenhardt L, Dupuy C, Groussin L, et al. Redifferentiation of radioiodine-refractory thyroid cancers. Endocr Relat Cancer. 2020;27:R113-R132.


46)) Cabanillas ME, Dadu R, Ferrarotto R, Liu S, Fellman BM, Gross ND, et al. Atezolizumab combinations with targeted therapy for anaplastic thyroid carcinoma (ATC). Journal of Clinical Oncology. 2020;38:6514-6514.

48)) Ou SI, Cui J, Schrock AB, Goldberg ME, Zhu VW, Albacker L, et al. Emergence of novel and dominant acquired EGFR solvent-front mutations at Gly796 (G796S/R) together with C797S/ R and L792F/H mutations in one EGFR (L858R/T790M) NSCLC patient who progressed on osimertinib. Lung Cancer. 2017;108:228-231.